Urinary Incontinence: Types, Causes, Symptoms, Diagnosis and Treatment

1. What is urinary incontinence?
2. How common is urinary incontinence?
3. What causes urinary incontinence?
4. What are the different types of urinary incontinence?
5. Why does urinary incontinence affect more women than men?
6. What are the risk factors of urinary incontinence?
7. What are the symptoms of urinary incontinence?
8. What are the complications of urinary incontinence?
9. How is urinary incontinence diagnosed?
10. How is urinary incontinence treated?
What is urinary incontinence?
The process of urination is controlled by various muscles of the urinary system. Important muscles for urination include the muscles of the urinary bladder and sphincter muscles of urethra. In the normal process, the urine is formed in kidneys and stored in the urinary bladder. When the bladder becomes full, the bladder muscle contracts, and there is a simultaneous relaxation of urethra muscles, which lead to urination. However, in some cases, there is a urine leakage due to poor control over the bladder function. This condition of leakage is known as urinary incontinence. During urinary incontinence, the muscle of bladder contracts suddenly, due to the pressure created by sneezing, laughing and exercising, and the sphincter muscles of the urethra are unable to withstand the pressure, thereby causing leakage of urine. Urinary incontinence is common in older people as compared to young people.
How common is urinary incontinence?
Because of its prevalence in approximately 5% of the general population, WHO has considered urinary incontinence as a social disease. The prevalence of urinary incontinence in various studies ranges from 5% to 70%. The prevalence increases with age. Approximately 40% of the women over the age of 70 years are affected by urinary incontinence. Females are more affected by urinary incontinence as compared to their male counterparts. The annual incidence of urinary incontinence is about 1% to 9%. Stress urinary incontinence was the most common cause followed by mixed urinary incontinence and urge incontinence.
What causes urinary incontinence?
Urinary incontinence may be either temporary or persistent.
Temporary urinary incontinence causes include:
- Food: Foods that stimulate the muscles of the bladder such as chocolate, artificial sweeteners, caffeine, alcohol, carbonated water, chilli or peppers, and citrus foods may also cause urinary incontinence.
- Constipation: Hard stool in the rectum may increase the frequency of urination.
- Urinary tract infection: Urinary tract infection may irritate the bladder leading to a strong urge for urination, painful urination, and urinary incontinence.
- Medications: Urinary incontinence may be caused due to various medications. These medications include diuretics used to treat hypertension, liver disease, and various kidney diseases.
Persistent urinary incontinence causes include:
- Urinary obstruction: When there is a blockage in the normal flow of urine either due to an enlarged prostate or a tumour due to stones, urinary incontinence may occur.
- Reduced control over bladder muscles: As the person ages, the involuntary contraction of bladder muscles increases. Further, control over bladder muscles also reduces with ageing.
- Pregnancy: During pregnancy, there is increasing pressure on the muscles of the urinary system due to increased fetal weight and hormonal changes. This may lead to urinary incontinence. Urinary incontinence may also be caused during childbirth due to damage of muscles required to control bladder activity.
- Surgery: Surgeries such as prostate surgery or hysterectomy may cause incontinence due to sphincteric damage or fistula formation respectively.
- Menopause: The muscular lining of the bladder and urethra are maintained by estrogen. During menopause, the level of estrogen reduces leading to poor functioning of these muscles.
- Neurological disorders: Neurological conditions such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis affects the nerve signals of the urinary system leading to urinary incontinence.
- Connective tissue disorders: Connective tissue disorder such as Ehlers-Danlos syndrome causes problems in the muscles of the urinary system.
- Overweight: The increased weight, especially of the tummy, put pressure on the muscles of the bladder and may cause urinary incontinence.
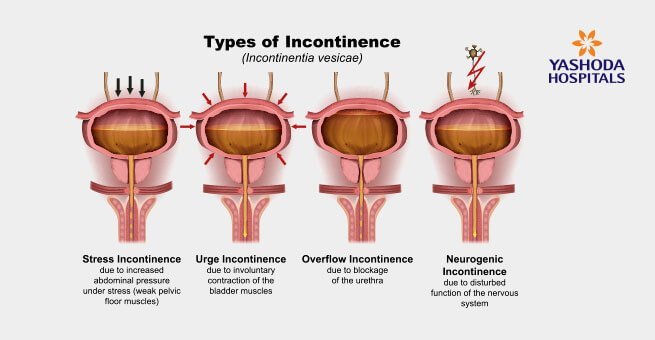
What are the different types of urinary incontinence?
Urinary incontinence type may help to evaluate the cause of urinary incontinence and deciding the precise treatment. The types of urinary incontinence are:
- Urge incontinence: In case of urge incontinence, there is a strong urge for urination, and the people are not able to hold the urine. This leads to involuntary flow or leakage of urine. The condition may be due to diabetes or neurological disorders.
- Stress incontinence: Thus occurs when there is an extra pressure on the bladder muscles due to exercise, laughing, lifting heavy objects, coughing or sneezing, and leakage of urine occurs. The condition is especially common in middle-aged women.
- Functional incontinence: In the case of functional incontinence, although the bladder function is normal the patient is unable to go to the toilet in time. This may be due to physical disability such as arthritis or mental disorder such as Alzheimer’s disease.
- Overflow incontinence: When a patient has significant post-void residual urine small volume of urine dribbles. This condition is caused due to enlarged prostate or spine injury leading to incomplete emptying of the bladder.
- Mixed incontinence: In some cases, the patient may suffer from more than one type of urinary incontinence.
Why does urinary incontinence affect more women than men?
Various health events specific to women make them more prone to urinary incontinence as compared to males. The pelvic floor muscles are important to control urination. However, pelvic floor muscles may damage due to pregnancy and childbirth. This may cause urinary incontinence. The urinary incontinence may also be caused due to menopause, a condition that is exclusive to women. During menopause, the level of estrogen reduces leading to poor health of the muscular lining of bladder and urethra. This causes poor control over urination.
Anatomical variations in women in comparison to men also cause urinary incontinence. For instance, shorter urethra in women makes them vulnerable to urinary incontinence.
What are the risk factors of urinary incontinence?
Urinary continence risk factors include:
- Overweight: Increased weight, especially on the abdominal area, increases pressure on urinary tract muscles leading to poor control over urination.
- Smoking and drinking: People who smoke and drink are at increased risk of developing urinary incontinence.
- Family history: A family history of urinary incontinence increases the risk of developing urinary incontinence.
- Gender: Specific conditions such as pregnancy, menopause, and childbirth, and a short urethra increase the risk of having urinary incontinence in the women.
- Age: As the age increases, control over bladder muscles reduces leading to urine leakage.
- Underlying medical conditions: Medical conditions such as prostatitis, BPH, prostate tumour, and neurological condition increase the risk of urinary incontinence.
What are the symptoms of urinary incontinence?
It is to be noted that urinary incontinence itself is a symptom of underlying medical conditions either leading to damaged urinary tract muscles or functional incontinence. Urinary incontinence symptom may be accompanied by:
- Increased urination frequency particularly at night (nocturia)
- Bedwetting
- Increased urge to urinate leading to spasm in the pelvic area
What are the complications of urinary incontinence?
Urinary incontinence, if left untreated, may lead to the following complications:
- Reduced quality of life: Urinary incontinence impacts the social, professional, and personal life of the patient. The patient avoids laughing, sneezing and coughing. It may sometimes lead to embarrassing situations.
- Increased incidence of urinary tract infection: Patients with urinary incontinence may have the problem of recurrent urinary tract infection. Further, catheters, when used for a prolonged period, may also cause urinary tract infection.
- Increased risk of skin diseases: Patients with urinary incontinence may develop skin sores, infections such as fungal infections, and rashes. Wound healing in such patients is also delayed.
How is urinary incontinence diagnosed?
Urinary incontinence diagnosis is done through the following techniques:
- Physical examination: The doctor physically evaluates the patient such as inspection of the strength of pelvic floor muscles in women and enlarged prostate in males.
- Urinalysis: Urinalysis is done to determine the presence of urinary tract infection, blood in urine, and other abnormalities.
- Postvoid residual (PVR) measurement: This test is done to determine the volume of urine present in the urinary bladder after urination.
- Urodynamic testing: This test evaluates the stress withstanding ability of bladder muscles and sphincter muscles.
- Stress test: During the stress test, the patient applies sudden pressure, and the doctor evaluates if there is any urinary leakage.
How is urinary incontinence treated?
Various options for urinary incontinence treatment are:
- Medications: Various medications are used to manage the symptoms of urinary incontinence. These medications manage overactive bladder and urge incontinence. Nerve stimulators and bulking material injections are also useful in managing urinary incontinence.
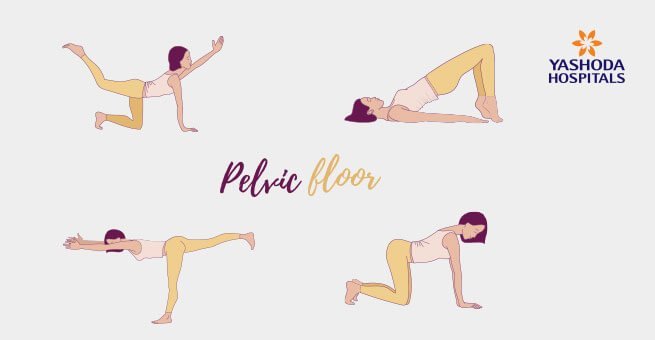
- Exercises: Exercises, such as pelvic floor muscle exercise, increase the strength of bladder muscles and sphincter muscles, and reduces stress incontinence.
- Devices: Pessary and urethral insert may help the women to manage urinary incontinence.
- Surgery: Surgical interventions for treating urinary incontinence include
- Sling procedures
- Prolapse surgery
- Bladder neck suspension
- Artificial urinary sphincter
- Behavioural techniques: Fluid and diet management, double voiding, and training for emptying bladder may help in managing urinary incontinence.
What is the Kegel exercise?
Kegel exercises are the exercises done to increase the strength of pelvic floor muscles. As the pelvic floor muscles support the uterus and urinary bladder, the exercise helps in managing symptoms of urinary incontinence. Exercise can also be done during pregnancy and prevent the weakening of pelvic floor muscles. You should consult with your healthcare provider before doing Kegel exercise.
How can urinary incontinence be prevented?
Measures for urinary incontinence prevention include
- Pelvic floor exercise: Urinary incontinence is generally due to the problems with bladder and urethra muscles. Pelvic floor exercises help to improve the strength of muscles thereby reducing the severity of urinary incontinence.
- Avoid smoking and drinking: Smoking and drinking results in an increased risk of urinary incontinence. With time, the smokers develop chronic cough which damages the pelvic floor muscles. Alcohol is a diuretic that increases the production of urine and increases urination frequency.
- Prevent constipation by eating dietary fibres: Constipation is one of the risk factors for urinary incontinence. Constipation increases the pressure on the bladder leading to urinary leakage. Chronic constipation also reduces bladder capacity.
- Managing weight: Obesity adds up to the severity of urinary incontinence. Increased adiposity on the abdominal area increases pressure on the bladder leading to urethral mobility. The overall process causes urine leakage.
- Avoid foods that stimulate bladder: The patient with urinary incontinence should take care of the kind of food consumed. Spicy foods, caffeine, artificial sweetener, chocolates, alcohol, and sodas increase urination. However, the patient should not reduce the intake of water as this may cause dehydration.
- Regular bathroom breaks: To avoid any urine leakage, the patient should have a regular bathroom break. This should be done even in cases when the patient does not feel the urge to urinate.
- Easy access to the bathroom: As urinary incontinence provides very little time to go to the bathroom before the urine leakage occurs, the patient should have easy access to the bathroom. The way to the bathroom should be clutter-free and well-lit all the time.
- Using absorbents: Absorbent pads should be used, especially in the elderly, to prevent the urine odour and risk of skin infection. Absorbent pads are designed to absorb the fluid and prevent the odour of urine.
- Underwear which is easy to get on and off: The undergarments should not be tight-fitted as this may exert extra pressure on the bladder and would be difficult to get off in case of urgent urination. The underwear should be such that it can be quickly removed.
- Take help: Like other medical conditions, urinary incontinence is also a health problem and the patient should not be embarrassed in getting help from the doctors as well as from family members. This is particularly important for people suffering from neurological disorders.
- Be prepared: Patients should always be prepared for a sudden episode of urine leakage and should always carry wipes, absorbents, and a set of clothes in case there is sudden urine leakage.
References:
- Urinary incontinence. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/urinary-incontinence/symptoms-causes/syc-20352808. Accessed on April 15, 2020.
- Urinary incontinence in older adults. NIH. https://www.nia.nih.gov/health/urinary-incontinence-older-adults. Accessed on April 15, 2020.
- Urinary incontinence. NHS. https://www.nhs.uk/conditions/urinary-incontinence/. Accessed on April 15, 2020.
- Urinary incontinence. Womenshealth.gov. https://www.womenshealth.gov/a-z-topics/urinary-incontinence. Accessed on April 15, 2020.











 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





