Pulmonary Endarterectomy: A Complex lifesaving lung surgery
Pulmonary Endarterectomy is a specialist surgical procedure for Pulmonary Hypertension resulting from a condition called Chronic Thromboembolic Pulmonary Hypertension (CTEPH). In the context of CTEPH, untreated pulmonary hypertension of >40mmHg has a poor prognosis with a 5 year survival of 30% and if the pulmonary pressure is >50 mmHg, then the 5 year survival is only 10%. The following describes what CTEPH is, how it presents, how it is diagnosed and what treatment options are available.

What is Chronic Thromboembolic Pulmonary Hypertension?
The term ‘Blood Pressure’ normally refers to the value of pressure in the arteries supplying blood to our bodies and typically measured by using an inflatable cuff around the upper arm. So, when someone has a high blood pressure, they are referred to as having ‘hypertension’ and being ‘hypertensive’. These arteries form the systemic circulation which is distinct from the arteries which supply our lungs, and which form the pulmonary circulation. A simple analogy of our circulatory system is that of a Figure-of-Eight racing track. The smaller loop involves the right ventricle, the heart pumping the dark or ‘blue’ blood into the lungs. Here the blood is loaded with oxygen before reaching the left side of the heart. The oxygen-rich ‘red’ blood then reaches the left side of the heart which pumps blood into the larger loop to supply the rest of the body. The pressure within the arteries of the pulmonary circulation can also be measured, either by estimation from an echocardiogram examination of the heart, or directly using an invasive catheter. When the pressure is high in these lung arteries, it is referred to as Pulmonary Hypertension (PH).
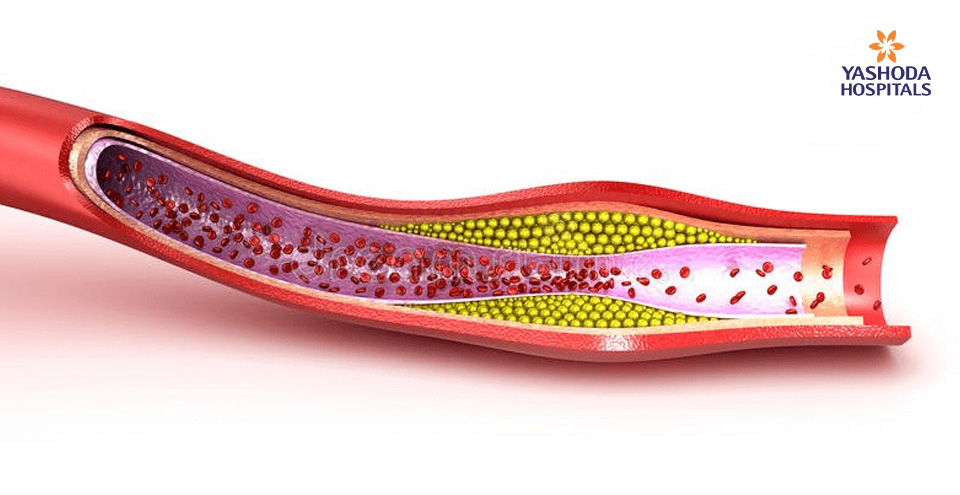
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is a relatively rare but potentially lethal and significantly underdiagnosed condition. It is one of many conditions that leads to PH and usually caused by blood clots or ‘thrombi’ (singular ‘thrombus’) which narrow or block one or more arteries in the lung. The blood clots arise from deep vein thrombosis (DVT) where some or all of the clotted blood within the deep veins, typically of the lower limbs, migrate or ‘embolize’ within the circulation to reach the lungs. This process called a Pulmonary Embolus (PE) is responsible for the majority of CTEPH cases. An estimated 800 individuals per million population will have a PE of which 4% will develop CTEPH and up to a quarter of them will benefit from a surgical procedure called Pulmonary Endarterectomy (PEA). If these blood clots, which stick to the internal walls of the pulmonary arteries, do not disappear on their own or following treatment with blood thinning medication, then the right ventricle struggles to pump blood into the lung circulation so that less oxygen is available for normal activity. This triggers the onset of symptoms. In time, these unresolved blood clots become organized into a chronic scar tissue and continue to restrict the normal flow of blood within the pulmonary circulation.
The diagnosis of CTEPH is confirmed once there is evidence of chronic clots within the pulmonary arteries despite 3 months of treatment with blood-thinning anticoagulant medication and the mean pulmonary artery pressure is equal to or more than 25 mmHg on a right heart catheter study with normal left heart function.

What risk factors are associated with CTEPH?
A number of diseases, some medical and surgical treatments as well as lifestyle and genetic factors are associated with the development of CTEPH. The most common causes are as follows:
- History of splenectomy (removal of the spleen)
- Presence of infected pacemaker leads
- Presence of ventriculo-atrial or ventriculo-peritoneal shunts which divert and drain excessive fluid from within the brain of patients with hydrocephalus to either the heart or the abdomen
- Immobility subsequent to trauma, surgery, or prolonged sedentary travel
- Hypothyroidism
- Chronic inflammatory diseases
- In the presence of cancer
- Use of the oral contraceptive pill
- Genetic factors that affect the normal blood clotting system in the body
What are the symptoms of CTEPH?
The symptoms associated with CTEPH also occur with other lung conditions. It is therefore not possible to make a diagnosis just on the basis of the presenting symptoms. The commonest complaints are of shortness of breath on exertion as well as fatigue and lethargy. Some patients also suffer from palpitations, fainting episodes, chest discomfort and infrequently the coughing up of blood- stained sputum or small amount of blood itself.

How is CTEPH investigated?
Your doctor will take a thorough medical history and perform a clinical examination which may reveal signs of pulmonary hypertension. A ventilation-perfusion scan is a necessary first screening test and if normal then it excludes a diagnosis of CTEPH. Additional CT or MRI scan of the lungs will demonstrate the presence of blood clots within the pulmonary circulation. An estimate of the pulmonary pressure can be made with a standard echocardiogram, but the exact figures and extent of the disease can only be made with a combination of a right heart catheter study as well as pulmonary and CT angiograms. The latter involve injecting some contrast dye in the circulation so that areas of narrowing and blockages within the arteries of the lungs are clearly demonstrated.

What treatment options are available for CTEPH?
The gold-standard and curative treatment for CTEPH is through a surgical procedure called Pulmonary Endarterectomy (PEA). However, some patients diagnosed with CTEPH have advanced disease that is not amenable to this surgical therapy. It is imperative that on diagnosis or on suspicion of the condition, patients are promptly referred to a specialist centre with multi-disciplinary expertise in the comprehensive evaluation and management of CTEPH. This includes specialists in radiology, pulmonary hypertension, in the surgical procedure and in post-operative intensive care. Early referral and assessment of operability ensures the best opportunity for a curative surgical procedure.
Even with surgery, a percentage of patients will have some residual disease that can be managed medically or by percutaneous intervention called Balloon Pulmonary Angioplasty (BPA). BPA is also recommended for CTEPH patients who are symptomatic but whose disease is not sufficiently extensive to warrant the risk of complex PEA surgery. Very few centres in the world have the necessary Interventional Radiology skills to perform BPA procedures for CTEPH.
CTEPH patients who are not suitable for surgery, BPA intervention, only have minimal or recurrent disease, are best served with medical management. Although there are numerous drugs which increase the diameter of the lung arteries (pulmonary vasodilators), only a single agent (a soluble guanylate cyclase stimulator) has been internationally approved as the evidence-based therapy for CTEPH. Medical management also includes mandatory life-long anticoagulation with Warfarin to prevent recurrence or further exacerbation of disease.

What is involved in Pulmonary Endarterectomy?
Pulmonary Endarterectomy (PEA), historically referred to as Pulmonary Thromboendarterectmy, is a complex surgical procedure that is a curative treatment for selected patients diagnosed with advanced CTEPH. Surgery involves general anaesthesia, a midline opening of the chest (sternotomy) as per most heart operations and the use of the heart-lung machine. As it is impossible to see through blood, the procedure requires cooling the body to 20℃ (deep hypothermia) and periods of circulatory arrest so that no blood is flowing. This technique of deep hypothermic circulatory arrest is a very safe and well established practice in cardiothoracic surgery. It permits excellent visualization of the disease so that all of the obstructive material can be removed to re-establish adequate blood flow in the pulmonary arteries. Sometimes, a portion of the disease that is very distal in the pulmonary arteries may not be amenable to PEA surgery. This results in some patients being left with a degree of residual disease and associated PH which may necessitate a combination of medical and BPA treatment.
The outcomes from PEA surgery depend on the degree of PH, the extent and distribution of the disease, as well as patient age and other concomitant medical conditions. In experienced centres with a focused CTEPH team, the immediate risk of surgery is under 5%. For those patients whose pulmonary pressures return to normal immediately after surgery, the outcome is excellent with a survival prognosis similar to peers of the same age in the community. When all high and low risk patients are grouped together, the expected survival following hospital discharge is around 90% at 5 years, 80% at 10 years and 60% at 15 years.
The key to CTEPH patients attaining the best medical management and long-term survival is through timely referral to a specialist centre. The referral should be made before initiating vasodilator therapy so that no time is lost in identifying those patients for whom surgery can be entirely curative with normal life expectancy.
References:
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH), Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/17635-chronic-thromboembolic-pulmonary-hypertension-cteph#. Accessed on 3rd March 2021.
- Chronic thromboembolic pulmonary hypertension (CTEPH), NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1955041/. Accessed on 3rd March 2021.
- PTE: Pulmonary Thromboendarterectomy Surgery for Pulmonary Hypertension, UC SanDiego Health, https://health.ucsd.edu/specialties/cardiovascular/programs/pulmonary-vascular-disease/pte/pages/default.aspx. Accessed on 4th March 2021.
- Pulmonary Thromboendarterectomy, Cleveland Clinic, https://my.clevelandclinic.org/health/treatments/21024-pulmonary-thromboendarterectomy-surgery. Accessed on 4th March 2021.











 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





