Pancreatic Cancer: Symptoms, Causes, Risk Factors, Diagnosis, Treatment
What is Pancreatic Cancer?
Cancer that occurs in the tissues of the pancreas is called Pancreatic Cancer. The pancreas is a vital endocrine organ located behind the stomach and plays an important role by producing enzymes that are required by the body to digest fats, carbohydrates and proteins and helps in the digestion of food.
- This vital organ produces important hormones like glucagon and insulin. These two hormones are mainly responsible for controlling glucose metabolism.
- Insulin helps the cells in metabolizing glucose to produce energy while glucagon helps in raising glucose levels when they are very low.
- Pancreatic Cancer is often diagnosed in the advanced stages of cancer as it can be difficult to detect due to the location of the pancreas.
What are the symptoms of Pancreatic Cancer?
Unfortunately, the signs and symptoms for Pancreatic Cancer don’t show up until the disease is at an advanced stage and hence there are no early signs or symptoms of this Cancer. Pancreatic Cancer that spreads can however worsen the preexisting symptoms like:
- Loss of appetite
- Unintended weight loss
- Jaundice
- Depression
- Abdominal pain that can radiate to the back
- Blood clots in Blood vessels
- Fatigue
- Itchy skin
- Light coloured stools (suggestive of obstructive Jaundice)
- Dark coloured urine (suggestive of obstructive Jaundice)
- Newly diagnosed diabetes or uncontrollable preexisting diabetes.

What causes Pancreatic Cancer?
The causes of Pancreatic Cancer are unknown. Pancreatic Cancer occurs when the abnormal cells in the pancreas begin to grow and form tumours.
- Usually, under normal conditions, healthy cells grow and die in moderate numbers whereas in a Cancer affected body there is an increase in the amount of abnormal cell production where these cells take over the healthy cells.
- The causes of these changes in the cells are not known yet, however, there may be some common factors that can increase the risk for a person to develop this type of cancer.
- Gene mutations and acquired gene mutations are the two most significant risk factors. A gene controls the way a cell acts and changes in those genes can lead to cancer.
Who is at risk?
Even though the cause for this type of cancer is not known yet, there are certain risk factors that can increase the chances for a person to develop Pancreatic Cancer. The person can be at risk if he :
- Smokes cigarettes – a fair percentage of Cancer cases are connected with cigarette smoking
- Obese
- Does not exercise frequently
- Eats fatty food
- Takes alcohol regularly
- Is diabetic
- Works with pesticides and chemicals
- Has a chronically inflamed pancreas
- Has a family history of Pancreatic Cancer or certain genetic disorders that can be linked to this type of Cancer.
DNA has a great influence on health and the conditions one may develop. A person can inherit genes that can increase the risk for Pancreatic Cancer.
How is Pancreatic Cancer diagnosed?
Although Pancreatic Cancer is discovered in the advanced stages, it is always best to consult the doctor if certain symptoms persist for longer durations.
To diagnose any medical condition or any symptom, the doctor reviews symptoms and the medical history of the patient. Depending on the symptoms tests may be ordered to confirm the diagnosis such as:
- A triphasic CT Scan or MRI is ordered to get a complete and detailed scan of the pancreas
- A biopsy or a tissue sample of the pancreas is ordered
- An endoscopic ultrasound, wherein a thin, flexible tube with a camera attached to it is inserted down into the stomach to obtain a clear image of the pancreas.
- Blood tests to detect the presence of tumour marker CA 19-9, which can indicate the presence of Pancreatic Cancer.
After the confirmation of diagnosis as Pancreatic Cancer, further tests are ordered to know to which extent the Cancer has spread.
- A PET scan helps the doctors in identifying if any Cancerous growths are present in the body. Blood tests are also referred to know the stage of Cancer it has advanced to.
- Identifying the stage of Cancer can help with the treatment options.
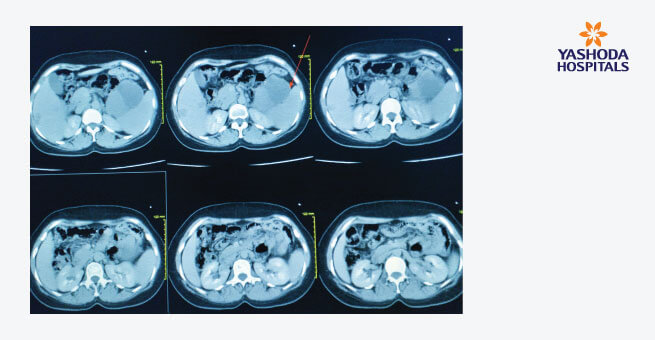
Once the doctor diagnoses, a stage is assigned based on the results of the test such as:
- Stage 1: the tumour exists within the pancreas only.
- Stage 2: the tumour has spread near the abdominal tissue or lymph nodes.
- Stage 3: Cancer has spread to the major blood vessels and the lymph nodes.
- Stage 4: The tumour has spread to the other organs, such as the liver.
How can Pancreatic Cancer be treated?
A Pancreatic Cancer can be cured only if it has been caught early which is rare and the majority of Pancreatic Cancer s are not found and diagnosed until the Cancer reaches the advanced stages and spreads beyond its original site.
- The treatment for Pancreatic Cancer entirely depends on the stage of the Cancer it has advanced to. The two goals of treating Pancreatic Cancer are to kill cells that are Cancerous and to prevent the disease from spreading further.
- Sudden weight loss, bowel obstruction, pain in the abdominal area and liver failure can be stated as some of the most common complications that occur during Pancreatic Cancer treatment.
The types of treatments involved in treating Pancreatic Cancer s are:
Surgery:
- Surgery can be recommended if the tumour is confined to the pancreas. The location of the Cancer determines whether surgery is an option or not as surgery can remove all or some portions of the pancreas.
- There are two types of surgeries that can be done: a Whipple procedure or a pancreatectomy.
- Pancreaticoduodenectomy also called a Whipple procedure is done to remove the tumours that are confined to the head and neck of the pancreas.
- Pancreatectomy is done to remove a portion or all of the pancreas, which eliminates the initial Cancer tumour but it is a very morbid procedure.
- Surgery is not recommended for advanced stages of Pancreatic Cancer. If cancer has advanced to the other parts of the body, removing the tumour or the pancreas will not cure the person and in such cases, other options of treatments are to be considered.
Radiation therapy:
This option can be considered when cancer has spread outside the pancreas. This radiation therapy uses high energy beams and X rays to kill the cancer cells.
Chemotherapy:
This option is considered as a combination with other treatments. Chemotherapy uses cancer-killing drugs to help prevent the future growth of cancer cells.
Targeted therapy:
This therapy involves treatment that uses drugs or other measures to target the Cancer cells specifically to destroy them. The drugs used in this therapy are not harmful to any healthy or normal cells.
How can Pancreatic Cancer be prevented?
As the causes of this Pancreatic Cancer are not known, this also means that the steps for prevention cannot be stated. However the gender, age and DNA cannot be changed but certain lifestyle changes can make a difference, such as
- Quitting smoking as it increases the risk for several types of Cancer s
- Reducing the intake of alcohol, as an increased intake can increase the risk for chronic pancreatitis and Pancreatic Cancer as well
- To maintain a healthy diet and weight, obesity is a leading cause of several types of Cancers.
Management of Pancreatic Cancer during COVID-19
- This type of cancer is very aggressive in nature and even if the treatment is done survival remains dismal.
- Managing patients with Pancreatic Cancer in the ongoing pandemic has become more complicated.
- COVID-19 has put the medical oncologists in a moral and ethical dilemma of whether to continue giving cytotoxic drugs which are at the risk of immunosuppression and predisposing already at high-risk patients to COVID-19 or to. hold the treatment with the risk of this progressive disease that already has a very poor prognosis, to begin with leading to an even poorer outcome.
- Managing these patients has become more difficult with limited experience in this rapidly evolving situation with no current guidelines available. It is imperative to come up with suggestions that can help to mitigate risks while at the same time can help the medical oncologists to come up with ways to continue treating Pancreatic Cancer patients safely.
- Cancer-stricken patients are generally at a higher risk of myelosuppressive effects of the treatment and the disease.
- COVID-19 infection also causes lymphopenia which can further weaken the immune system.
- It is very important for a medical oncologist to strongly weigh the risks versus the benefits of continuing cytotoxic treatments for Pancreatic Cancer patients in the ongoing pandemic as the patients who underwent chemotherapy or surgery in the ongoing pandemic had severe events when compared to patients who did not receive any treatment.
To prioritize the treatments for patients with Cancer during this pandemic, they can be divided into three groups :
- Group A: Patients who have completed their treatment or the disease is under control
- Group B: Patients who still are undergoing active treatment such as adjuvant or neoadjuvant with curative intent.
- Group C: Patients with metastasized disease undergoing treatment.
For Group A it is recommended to delay the consultation visits and follow up appointments and use telemedicine visits instead of a physical consultation.
For Group B it is recommended to treat a Cancer patient within a COVID-19 free clinical pathway that can reduce the risk of COVID-19 infection to all the patients by following the universal guidelines of washing hands, social distancing and wearing personal protective equipment.
For Group C it is recommended to delay the treatment if not compromise disease control. If the decision to continue the treatment is taken then the COVID-19 free clinical pathway can be recommended.
For oral therapy, the doctor should provide drug supply for 2-3 courses along with home monitoring and using telemedicine for toxicity management.
Conclusion
- Cancer-stricken patients are at increased risk of having a poor outcome due to the ongoing global pandemic situation and are considered a high-risk group.
- The present data suggests adverse events, complications and even death from COVID-19 was reported.
- Pancreatic Cancer is a very aggressive disease and even if treated the outcome still remains poor.
- It is very challenging to take care of Pancreatic Cancer patients in the ongoing pandemic as the decision to treat or not to treat becomes almost impossible.
- The goal is to protect the vulnerable population and at the same time not to compromise on survival or disease control.
- A medical oncologist should use an individualized treatment strategy to decrease the frequency of clinical visits by using telemedicine for toxicity management.
References:
- Pancreatic Cancer, Mayo clinic: https://www.mayoclinic.org/diseases-conditions/pancreatic-Cancer /diagnosis-treatment/drc-20355427
- Pancreatic Cancer, Healthline: https://www.healthline.com/health/pancreatic-Cancer
- Pancreatic Cancer during covid-19, NCBI: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7201379/
About Author –
Dr. K. Sreekanth, Consultant Surgical Oncologist, Yashoda Hospital, Hyderabad
MS, M.Ch (Surgical Oncology)








 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





