Navigating Pancreatic Cancer: FAQs and Facts You Need to Know
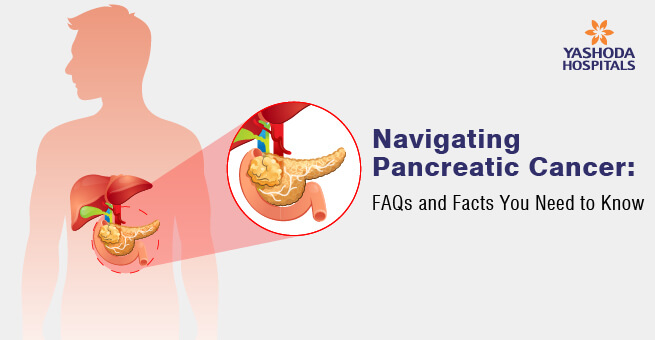
Pancreatic cancer, although relatively rare, carries significant challenges due to its often late detection and aggressive nature. Understanding its symptoms, risk factors, and available treatments is crucial for both patients and their families. In this comprehensive guide, we’ll address frequently asked questions about pancreatic cancer, dispel common myths, provide crucial facts, and offer insights to empower individuals in their journey against this disease.
Understanding Pancreatic Cancer: FAQs and Insights
What are the common symptoms of pancreatic cancer?
Pancreatic cancer symptoms show up late and can be easy to miss. Pay attention to signs such as persistent upper abdomen (belly) and/or middle or upper back pain, yellowing of the skin or eyes (jaundice), unexplained weight loss, and ongoing digestive issues. If you notice these signs, it’s essential to seek medical advice promptly.
Is pancreatic cancer likely to spread quickly?
Once pancreatic cancer develops, it has a tendency to spread rapidly to different parts of the body, underscoring the importance of early detection. Pancreatic cancer diagnosis in its early stages enables doctors to intervene promptly and potentially improve treatment outcomes.
What are the different pancreatic cancer stages?
Pancreatic cancer is classified into four stages. In the early stages (I and II), the tumor is confined to the pancreas. As it progresses to stage III, it extends beyond the pancreas, possibly involving nearby blood vessels. In the advanced stage (IV), the cancer spreads to distant organs, making treatment more challenging. Identifying the stage helps determine the treatment approach and prognosis.
What symptoms indicate that your pancreas has spread to other parts of your body?
When pancreatic cancer spreads to other parts of the body, you may experience unexpected changes in your health or symptoms related to other organs. These signs could suggest that the cancer has spread beyond the pancreas, and it’s essential to discuss any new or concerning symptoms with your doctor for further evaluation and guidance.
How do doctors determine whether pancreatic cancer has spread?
Pancreatic cancer tests include imaging scans (CT, MRI, PET), biopsies, and blood tests that aid doctors in determining if pancreatic cancer has spread. These evaluations provide detailed insights, helping doctors understand if the cancer has reached other parts of the body, assess the extent of the cancer’s spread, and guide them in planning the most effective treatment for the patient’s specific situation.
How is pancreatic cancer treated once it has spread to other parts of your body?
When pancreatic cancer spreads, treatment focuses on managing symptoms and improving quality of life. Options include chemotherapy, targeted therapy, radiation, or medications to alleviate discomfort. The goal is to enhance comfort and well-being, even though curing the cancer might be more challenging at this stage.
Is there a vaccine available for pancreatic cancer?
While no specific vaccine is currently available, ongoing research aims to develop vaccines and better medications, as well as improved surgical techniques for pancreatic cancer, offering hope for future advances in the fight against this disease.
Is pancreatic cancer hereditary?
Pancreatic cancer might occur in families at times, but it often arises without a clear hereditary connection. While family history can play a role, factors like smoking, age, and obesity also contribute significantly.
Who is at risk for pancreatic cancer and what causes it?
Pancreatic cancer risk factors include smoking, family history, obesity, and advancing age. While some cases have genetic links, most arise due to lifestyle and environmental factors. However, the exact cause of each case might vary. Regular health check-ups and adopting a healthy lifestyle can help manage potential risks and aid in pancreatic cancer prevention.
How to lower the risk of pancreatic cancer?

To lower the risk of pancreatic cancer, consider lifestyle changes such as adopting a balanced diet, quitting smoking, maintaining a healthy weight, and moderating alcohol intake. Regular physical activity and effectively managing chronic conditions like diabetes could further diminish the risk. Engaging in discussions with healthcare providers about concerns and embracing a healthy lifestyle play vital roles in significantly reducing the likelihood of developing pancreatic cancer.
What are the different types of pancreatic cancer?
Pancreatic cancer primarily includes two main types: adenocarcinomas and neuroendocrine tumors. Adenocarcinoma is the most common form, arising from gland cells. Neuroendocrine tumours, which are less common, grow from hormone-producing cells. Both have various subtypes with different symptoms and outcomes, requiring unique diagnostic and treatment approaches guided by healthcare providers’ detailed assessments.
How do doctors differentiate between different types of pancreatic cancer?
Medical experts distinguish between different types of pancreatic cancer by examining tissue samples obtained through biopsies. These samples undergo detailed microscopic analysis and specialized tests to identify specific cell types and genetic features. Additionally, imaging scans like CT or MRI help understand tumor characteristics, aiding doctors in accurately identifying the specific type of pancreatic cancer for personalized treatment strategies.
How are different types of pancreatic cancer treated?
The treatment for different types of pancreatic cancer varies based on the type and stage of the cancer and may include surgery, radiotherapy, chemotherapy, targeted therapy, or a combination of these. While benign pancreatic tumors (non-cancerous) may not require aggressive treatment and can be managed through observation or surgery, cancerous tumours that have spread to pancreatic lymph nodes and other organs may require surgery or other therapies, depending on the cancer’s progression and the patient’s health.
What is the most aggressive form of pancreatic cancer?
The most aggressive form of pancreatic cancer is typically adenocarcinoma. It is known for its rapid spread and detection at later stages, posing significant treatment challenges. Early identification remains crucial for better managing this type of cancer.
How to diagnose pancreatic cancer early?
Early diagnosis involves being attentive to symptoms like pancreatic cancer pain, which often presents as persistent abdominal and lower back pain, as well as other symptoms such as jaundice, unexplained weight loss, and digestive issues. Consulting a healthcare professional about persistent symptoms or health concerns is crucial for timely evaluation and the potential early detection of pancreatic cancer.
Can ultrasound detect pancreatic cancer?
Yes, ultrasound can help detect pancreatic cancer by creating images of the pancreas. There are two types of ultrasounds used for pancreatic cancer detection, abdominal and endoscopic ultrasounds, which help visualize the pancreas for potential signs of cancer. However, while it’s useful, sometimes additional tests like CT scans or MRIs might be needed for a more accurate diagnosis.
What is pancreatic cancer life expectancy and prognosis?
The prognosis for pancreatic cancer varies widely and is often challenging, with lower survival rates compared to other cancers. Factors like the stage of diagnosis, treatment response, overall health, and the availability of effective pancreatic cancer medications greatly influence life expectancy. Though advancements in treatments offer hope, detecting the disease early significantly improves overall outcomes.
When should you consult a doctor?

If you experience persistent symptoms like abdominal pain, unexplained weight loss, jaundice (yellowing of the skin or eyes), or digestive issues, it’s crucial to consult a doctor promptly. Additionally, if you have concerns about your health or notice any unusual changes that persist, seeking medical advice early ensures timely evaluation and appropriate guidance for any potential health issues.
Did you know that 4th stage pancreatic cancer has a five-year survival rate of 1-3 percent?
Dispelling Common Myths About Pancreatic Cancer
Myth 1: Pancreatic Cancer is Contagious
Contrary to common belief, pancreatic cancer cannot spread from person to person through contact. It’s important to know that cancer, including pancreatic cancer, is not contagious.
Myth 2: Pancreatic Cancer is Asymptomatic
In its early stages, pancreatic cancer may not show noticeable symptoms, making early detection challenging. However, it can lead to symptoms like abdominal pain, jaundice, weight loss, and digestive issues as it progresses. These symptoms become more pronounced in the last stages of pancreatic cancer.
Myth 3: Only People with a Family History Develop Pancreatic Cancer
While a family history of pancreatic cancer can increase the risk, most cases occur without a clear hereditary link. Also, not everyone who has a family history of the disease will develop it.
Myth 4: Pancreatic Cancer is an Older Person’s Disease
Although age is a risk factor, pancreatic cancer can affect individuals of any age group. It is not a disease that only affects the elderly.
Myth 5: Diabetic Patients Always Develop Pancreatic Cancer
Long-term diabetes can be a significant risk factor for pancreatic cancer, but not everyone with diabetes develops pancreatic cancer. It is critical to understand that diabetes is more likely to be a symptom and a potential risk factor than the direct cause of pancreatic cancer.
Myth 6: Pancreatic Cancer Screening Tests are Readily Available
Unlike some other cancers, there isn’t a widely recommended screening test for pancreatic cancer for the general population. It’s crucial to recognize symptoms and discuss concerns with healthcare providers.
Conclusion
In navigating the complexities of pancreatic cancer, separating myths from facts becomes imperative. Through this guide, we’ve shed light on common misconceptions along with frequently asked questions while providing vital information to aid in recognizing symptoms, understanding risk factors, and exploring available treatments.
Remember that early detection, making informed decisions, and ongoing discussions with healthcare providers are the cornerstones of dealing with pancreatic cancer. By embracing facts, we equip ourselves to better comprehend this challenging illness and strive for improved outcomes and well-being.
References:
- Pancreatic Cancer Symptoms https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-symptoms
- What are the Signs that Pancreatic Cancer Has Spread to Other Parts of Your Body? https://www.healthline.com/health/pancreatic-cancer/signs-that-pancreatic-cancer-has-spread
- Pancreatic Cancer Types https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer
- Pancreatic Cancer Diagnosis https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-diagnosis
- Treatment Types https://pancan.org/facing-pancreatic-cancer/treatment/treatment-types/
- What are the Different Types of Pancreatic Cancer? https://www.healthline.com/health/pancreatic-cancer/types-of-pancreatic-cancer#neuroendocrine
- Pancreatic Cancer Prognosis https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-prognosis
- Pancreatic Cancer Stages https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-stages
- 7 Myths And Facts About Pancreatic Cancer That You Need To Know For Good https://www.onlymyhealth.com/myths-facts-about-pancreatic-cancer-1641536913
- Pancreatic cancer fact-check https://www.baptistjax.com/juice/stories/cancer/pancreatic-cancer-fact-check
- Myth Or Fact: What You Need To Know About Pancreatic Cancer https://www.gutcare.com.sg/myth-or-fact-what-you-need-to-know-about-pancreatic-cancer/
About Author –
MS (General Surgery), DNB (Surgical Gastroenterology), FALS (Oncology)








 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





