Mediastinal Lymphadenopathy
Did you know that mediastinal lymphadenopathy affects millions of people worldwide? According to studies, a majority of patients with lung cancer and lymphoma develop mediastinal lymphadenopathy. This complex condition can have various underlying causes, ranging from infections to cancer. However, with the right information and support, it’s possible to successfully manage mediastinal lymphadenopathy and achieve a positive outcome. In this blog, we’ll explore the causes, symptoms, diagnosis, and treatment of mediastinal lymphadenopathy, as well as the new technique of EBUS-TBNA for diagnosis.
What is mediastinal lymphadenopathy?
Mediastinal lymphadenopathy is a condition characterised by the abnormal enlargement of lymph nodes in the mediastinum, which is the central part of the chest cavity located between the lungs. The mediastinum contains several vital structures, including the heart, trachea, oesophagus, and large blood vessels, as well as the lymph nodes of the central chest.
Enlarged mediastinal lymph nodes can be a symptom of various medical conditions, such as lower respiratory tract infections and cancer. The condition can be benign or malignant and can present with a variety of symptoms, including chest pain, shortness of breath, and a persistent cough.
What are the symptoms of mediastinal lymphadenopathy?
The symptoms of mediastinal lymphadenopathy can vary depending on the underlying cause and the severity of the condition. Some common symptoms include:
- Chest pain or discomfort
- Shortness of breath
- Persistent cough
- Wheezing
- Difficulty swallowing
- Hoarseness
- Swelling of the face, neck, or arms
- Fatigue
- Night sweats
- Fever
- Weight loss
What are the causes of mediastinal lymphadenopathy?
Mediastinal lymphadenopathy causes include various medical conditions. Some of the common causes are:
- Malignancy: Lymphoma, multiple myeloma, Castleman’s disease, leukaemia, lung cancer, lymphangitis carcinomatosis , kaposi sarcoma and other types of cancer can cause enlargement of the mediastinal lymph nodes.
- Benign causes:
- Infections: Infections such as tuberculosis, fungal infections, non tuberculous mycobacteria, histoplasmosis, coccidioidomycosis and bacterial infections can cause enlargement of the mediastinal lymph nodes.

- Inflammatory diseases: Inflammatory diseases such as sarcoidosis, chronic beryllium disease, rheumatoid arthritis and Crohn’s disease can cause inflammation of the lymph nodes and lead to enlargement.
- Infections: Infections such as tuberculosis, fungal infections, non tuberculous mycobacteria, histoplasmosis, coccidioidomycosis and bacterial infections can cause enlargement of the mediastinal lymph nodes.
What are the methods of diagnosing mediastinal lymphadenopathy?
Mediastinal lymphadenopathy can be diagnosed through a variety of methods, as it is usually not visible or palpable from the outside. Here are some common diagnostic methods:
- Imaging Tests
Imaging tests are non-invasive procedures used to assess the size, number and position of lymph nodes in the chest. CT scans are more sensitive than chest X-rays. Contrast enhanced computed tomography (CECT) of the chest is the initial investigation. PET CT is more sensitive and specific than CE CT chest for assessment of mediastinal lymph nodes and staging of lung cancer and other metastatic cancers, but it has a minor role in other benign disease conditions. - Sampling
If the cause of mediastinal lymphadenopathy is uncertain, a biopsy may be necessary to identify the underlying condition. The most common procedure is mediastinoscopy, a surgical procedure that involves a small incision above the sternum to insert a fibre-optic instrument called a mediastinoscope to obtain a sample of one or several lymph nodes. Another less invasive procedure, fine needle aspiration (FNA), either endobronchial or esophageal ultrasound , can also be done to obtain a biopsy sample. Rarely, thoracoscopy and anterior mediastinotomy can also be considered for sampling of mediastinal lymph nodes. - Mediastinoscopy
A mediastinoscopy is a surgical procedure that examines the mediastinum, the space in the chest between the lungs. The procedure involves making a small cut above the clavicular heads and inserting a scope to check the lymph nodes in the chest. If any abnormalities are noticed, they will be biopsied. Mediastinoscopy is usually performed under general anaesthesia in a hospital setting.
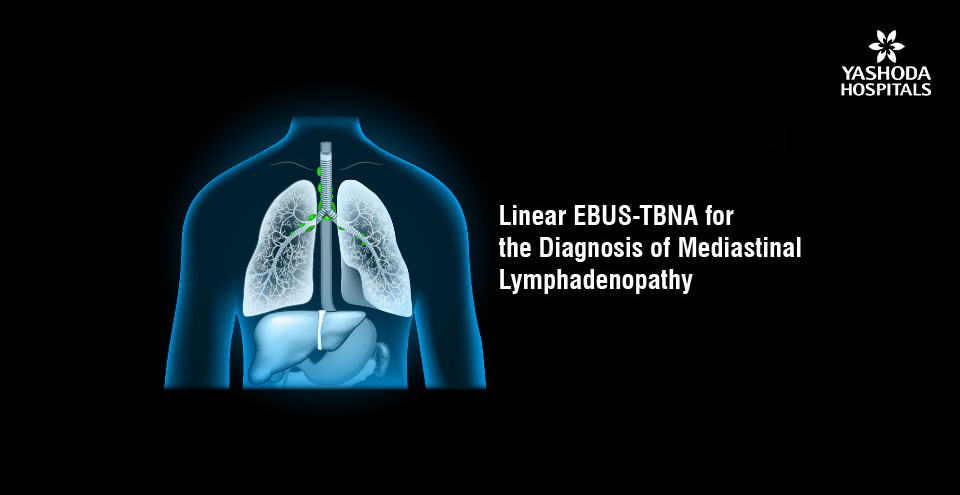
Linear EBUS TBNA for the diagnosis of mediastinal lymphadenopathy
Linear EBUS-TBNA is a minimally invasive diagnostic procedure commonly used to obtain samples from mediastinal lymph nodes in patients with mediastinal lymphadenopathy.
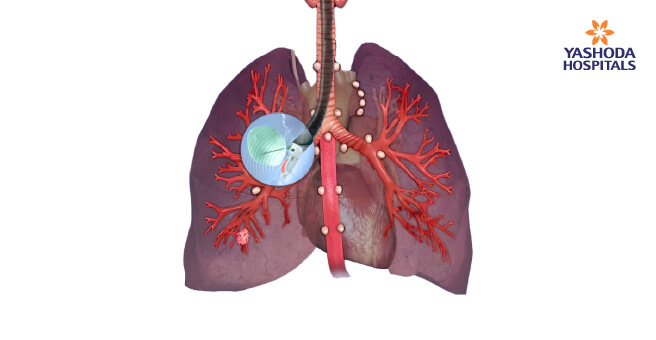
EBUS-TBNA combines endoscopic visualisation of the mediastinal lymph nodes with high-frequency ultrasound (USG) imaging and also enables the obtaining of cytological and histological samples of lesions.
During the procedure, the patient is usually sedated but awake, and a flexible bronchoscope with an ultrasound probe at its tip is inserted through the patient’s mouth and passed down to the level of the lymph nodes. The ultrasound probe creates images of the mediastinal structures and lymph nodes on a monitor, which the doctor uses to identify the most appropriate lymph node for sampling. A long, thin needle is then passed through the bronchoscope and into the lymph node to collect a sample of cells or tissue for analysis.
EBUS-TBNA has several advantages over other diagnostic procedures. It is less invasive than surgical biopsy procedures, such as mediastinoscopy, which can require general anaesthesia and a hospital stay. EBUS-TBNA tests can be performed on an outpatient basis, which can be more convenient and less expensive for patients.
EBUS-TBNA also has a high diagnostic yield, with a sensitivity and specificity of up to 90% and 100%, respectively, for the diagnosis of mediastinal lymphadenopathy. Additionally, EBUS-TBNA allows for accurate and minimally invasive sampling of mediastinal lymph nodes, which can provide a definitive diagnosis and guide appropriate treatment.
EBUS-TBNA enables access to a wide range of mediastinal and hilar lymph nodes and lesions around the airways. It is also useful for both the diagnosis and staging of lung cancer. In patients with suspected lymphoma and cases where more tissue is needed for molecular analysis, a newer approach called EBUS-transbronchial cryonodal biopsy may be considered.
What is the treatment for mediastinal lymphadenopathy?
The mediastinal lymphadenopathy treatment depends on the underlying cause of the condition. In some cases, the lymph nodes may shrink on their own without treatment, while in other cases, medical intervention may be necessary.
- Observation and monitoring: If the lymphadenopathy is mild and the cause is benign, the doctor may recommend a wait-and-watch approach, with regular monitoring of the lymph nodes to ensure that they are not growing or causing any symptoms.
- Medications: The doctor may prescribe the medicines based on the underlying causes. In cases where the causes are benign like tuberculosis and fungal infections the doctor may prescribe antitubercular and antifungal medicines.
- Radiation therapy: In cases where lymphadenopathy is caused by cancer, radiation therapy may be used to shrink the cancerous cells.
- Chemotherapy: Chemotherapy, which uses drugs to destroy cancer cells, may be recommended for lymphoma or other types of cancer that have spread to the mediastinal lymph nodes.
- Surgery: In some cases, surgery may be required to remove the enlarged lymph nodes or to biopsy them to determine the underlying cause.
Lastly, receiving a diagnosis of mediastinal lymphadenopathy can be a daunting experience. This complex condition can have a range of underlying causes, from infections to cancer, and diagnosis requires thorough evaluation. However, there is hope. EBUS-TBNA has emerged as a promising and less invasive tool for diagnosis, and with early detection and appropriate treatment, the outlook can be favourable. It is advised to seek immediate medical attention if you are diagnosed with mediastinal lymphadenopathy for further evaluation and management. Many people successfully manage their conditions, so don’t be afraid to take an active role in your healthcare and stay positive.
References:
- Mediastinal Lymphadenopathy
https://www.verywellhealth.com/mediastinal-lymph-nodes-2252159 - What is mediastinal lymphadenopathy?
https://www.medicalnewstoday.com/articles/mediastinal-lymphadenopathy - The role of Endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA) for qualitative diagnosis of mediastinal and hilar lymphadenopathy: a prospective analysis
https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-11-100 - Endobronchial Ultrasound for the Diagnosis and Staging of Lung Cancer
http://sleepdrs.com/wp-content/uploads/2015/09/doc1.pdf - Surgical Evaluation of Mediastinal Lymphadenopathy
https://www.uptodate.com/contents/surgical-evaluation-of-mediastinal - Hürter T, Hanrath P. Endobronchial sonography: feasibility and preliminary results.
https://thorax.bmj.com/content/47/7/565 - Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer
https://europepmc.org/article/MED/20740503
About Author –
Dr. Sathish C Reddy. S,Consultant Interventional Pulmonologist, Yashoda Hospitals
MD, DM Pulmonology (AIMS)









 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





