What is Minimally invasive spine surgery (MISS)?
At a Glance:
1. What is Full Endoscopic Spine Surgery (FESS)?
2. What are the conditions treated with Full Endoscopic Spine Surgery (FESS)?
3. What are the common endoscopic spine surgery treatment options?
4. Who are suitable candidates for Full Endoscopic Spine Surgery (FESS)?
5. What are the benefits of Full Endoscopic Spine Surgery (FESS)?
6. Is Full Endoscopic Spine Surgery (FESS) safe – what are the risks?
7. Recovery after Full Endoscopic Spine Surgery (FESS), how long does it take?
8. How should one choose a facility for Full Endoscopic Spine Surgery (FESS)?
What is Minimally Invasive Spine Surgery (MISS) and Full Endoscopic Spine Surgery (FESS)?
Full Endoscopic Spine Surgery (FESS) is the least invasive and very effective surgical technique to treat sliped or prolapsed disc.
Minimally invasive spine surgery (MISS) is a surgical procedure for the backbone or the bones of the spine. The term “minimally invasive” signifies that the surgery is carried out using much smaller cuts or incisions as compared to the standard, open surgery where the incisions are typically long, and go down the back. Surgery of the spine is often recommended as a second line of treatment for back problems once the more conservative approaches, i.e. medications or physical therapy fail to bring about the desired outcomes.
Open surgery is more traumatic not only due to the size of the incision but also because there is considerable harm to the nearby tissues and muscles as they need to be moved away for visualization of the surgical field and instrumentation. On the contrary, because of the reduced trauma to the muscles and soft tissues due to a smaller incision, minimally invasive surgical procedure is faster, safer and has a reduced recovery time.
While in some cases, the size of incision primarily defines whether surgery is minimally invasive, in such a case MISS may only be a description of the incision whereas the actual surgical procedure may still be the same. In a majority of cases of “minimally invasive” techniques a series of tubes known as “tubular retractors”, going from smaller to larger are used to stretch and retract the soft tissues for the surgical exposure.
The size of the tubular retractor is governed by two factors:
- The amount of light required to visualize the surgical site
- The size of the instruments required to perform the surgical procedure.
The size of the tubular retractor, in turn, determines the size of the incision or the extent of invasiveness. Usually, the smaller the diameter of the tube, the lesser invasive is the procedure, but more is the skill required to perform the procedure.
Minimally invasive surgery is recommended in certain cases of degenerative discs, fractures and herniated disc kyphosis, infection, scoliosis and spinal column tumours. Some of the commonly performed minimally invasive spine surgery procedures are:
- Correction of deformities such as for kyphosis and scoliosis
- Decompression of spinal tumours
- Repair and stabilization of fractures of vertebral compression
- Repair of herniated discs
- Spinal fusion for degenerative discs
At present, “Endoscopic spine surgery” (ESS) is the least invasive spine surgery which is performed with the smallest tubes in the range of 3mm –10mm for different procedures and an incision of few millimetres. Endoscopic spine surgery is performed with a tube fitted with a high definition camera that allows the surgeon to get to and visualize the pathology without causing much collateral damage to surrounding tissues. Since the light source is located at the tip of the instrument, the need to shine a light from the access point is eliminated, creating an opportunity to reduce the size of the tube.
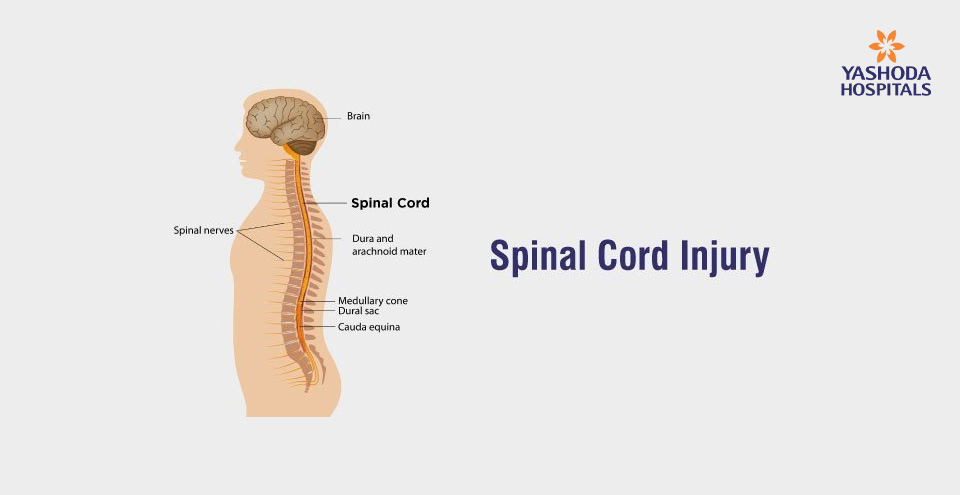
What are the conditions treated with Full Endoscopic Spine Surgery (FESS)?
Endoscopic spine surgery may be suitable for a large number of painful conditions of the spine. Some of the commonly treated conditions using endoscopic techniques are:
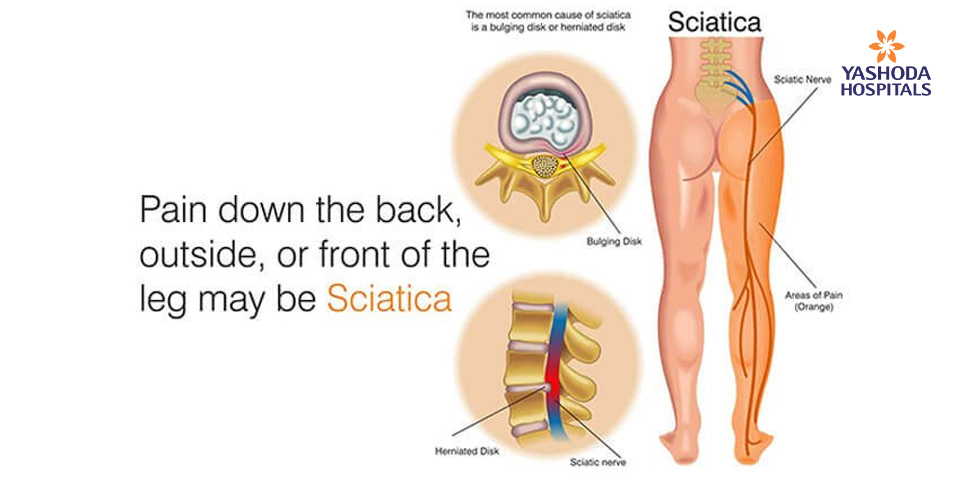
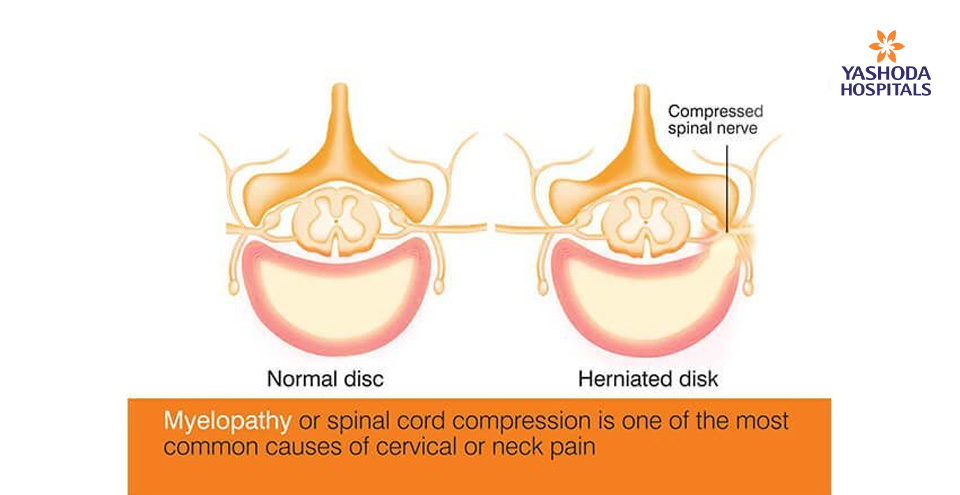
- Herniated, protruded or prolapsed disc – Inner portion of the disc protrudes through the outer ring causing numbness and pain
- Recurrent disc herniations – Herniated disc material at the same level in a patient who has undergone discectomy
- Degenerative spine diseases – Age related breakdown of one or more spinal discs leading to pain
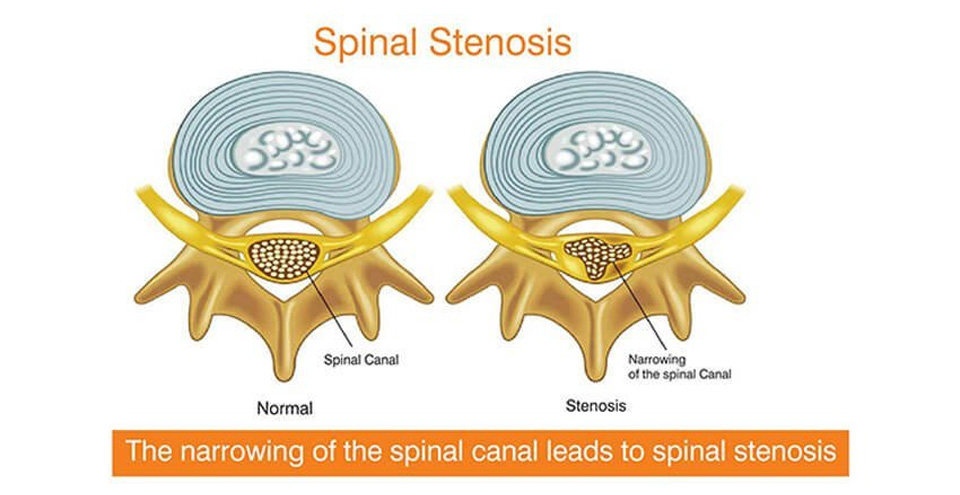
- Spinal canal stenosis – Narrowing of spinal canal both lateral and central
- Facet syndrome or Facet hypertrophy – Degeneration and enlargement of the facet joints
- Annular tears – Tear or rupture anywhere around the disc
- Failed back syndrome – Chronic pain following back surgeries
- Discitis – Inflammation between the intervertebral discs of your spine
- Spinal tumors – Benign (non-cancerous) or malignant (cancerous).
- Adjacent level disease after spinal fixation
- Spine listhesis – One of the bones of the spine (vertebrae) slips out of place onto the vertebra below it
In most cases, the major goals of the surgery are to relieve the affected nerve root from pressure or irritation or to interrupt the pain sensations from the sensory nerves.
What are the common endoscopic spine surgery treatment options?
Today, the endoscopic technique may be applied for many types of spine surgery with faster recovery time and fewer risks of developing complications. The undermentioned procedures are performed commonly:
- Decompression: A procedure to remove the pathology/structure causing pressure on a nerve
- Fusion: A procedure in which two or more vertebrae (smaller bones that form the building blocks of the spine) are joined or fused into a single, solid bone to eliminate painful motion or to restore stability to the spine.
- Disc Replacement: Pain relief is achieved by removal of the painful disc and placement of a prosthetic implant to maintain the motion at that spinal segment.
- Rhizotomy: Division of the sensory nerve that produces pain
- Foraminotomy: The nerves of the spinal cord exit through a small opening known as intervertebral foramen which is located between the vertebrae. In certain conditions, these openings may become too small and compress the nerve. In such a case, endoscopic lumbar and cervical foraminotomy may be done to relieve pressure on compressed nerves by enlarging the area around one the affected bones in the spinal column.
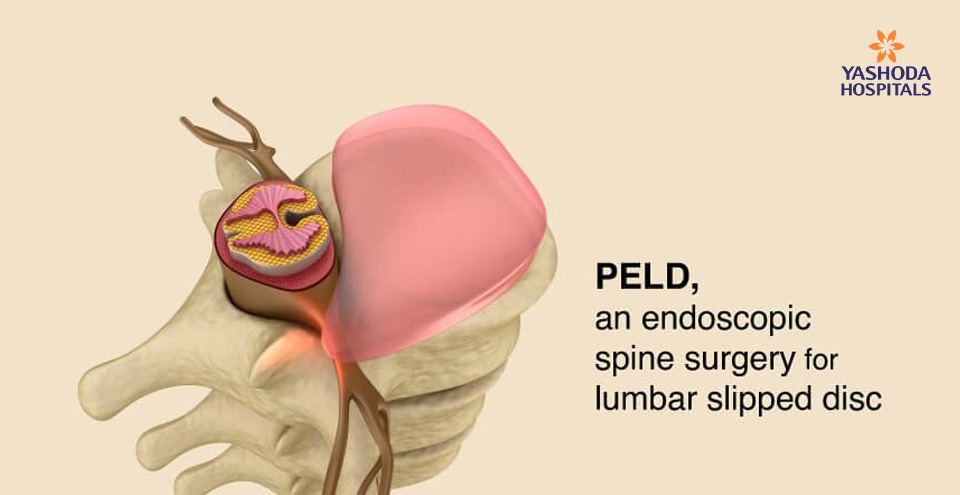
- Discectomy: Selective Endoscopic Discectomy (SED) or endoscopic discectomy is an endoscopic spine surgery treat problems of the disc that cause back and leg pain. A Micro Endoscopic Discectomy is an endoscopic procedure performed to relieve pain caused by a herniated disc which is pressing on a nerve root.
- Balloon kyphoplasty: This is a type of endoscopic spine surgery done for the treatment of spinal fractures caused by conditions like osteoporosis.
What are the common Full Endoscopic Spine Surgery options?
Transforaminal endoscopic procedures
- Thoracic or lumbar discectomy – removal of affected disc (whole or partial)
- Foraminoplasty – relieve pressure on compressed nerves
- Annuloplasty – cauterize outer compressing portions of the disc wall
- Aspiration of epidural abscess – removal of infected material
- Spinal fusion – fusing the affected spinal joints
Interlaminar endoscopic procedures
- Discectomy – removal of affected disc (whole or partial)
- Decompression of lateral recess stenosis
- Decompression of central canal stenosis
Endoscopic posterior foraminotomy and cervical discectomy to relieve pressure on compressed nerve and remove affected disc
Endoscopic visualized rhizotomy to sever nerve roots in the spinal cord
Who are suitable candidates for endoscopic spine surgery?
One of the most important steps to successful endoscopic spine surgery is an appropriate diagnosis.Even though many candidates for endoscopic spine surgery have common types of spinal disorders like facet arthropathy, moderate to severe disc herniation, sciatica, and spinal stenosis, spine surgery is not always considered to be the first line of treatment. Non-surgical options like spinal injections and physical therapy is considered before any type of spine surgery is advised.
Some of the variables that influence successful surgical outcomes include:
- Nature of pain and symptoms: Typically, history of pain that radiates from the back to the arm or leg, suggesting a nerve compression. Similarly, origin is more likely to have better outcomes in comparison to a chronic, long-standing condition.
- Individual’s lifestyle: Individuals leading an active, healthy lifestyle with regular physical exercise are more likely to have positive surgical outcomes.
- Smoking and personal habits: Tobacco consumption in the form of smoking causes decreased blood flow to various organs and body parts, including the spine. Consequently, the discs of the spine start degenerating and weakening of bones also occurs. The inhibitory effect of tobacco on healing may also pose to be a problem during healing spinal fusions and may also lead to the slowing of the overall healing process.
- Obesity: Overweight or obese people often face back problems and pain due to excessive strain on their back muscles. Surgery may not be always a suitable option for such individuals as they are also more prone to complications after spine surgery. However, this doesn’t imply that no obese person can undergo minimally invasive or endoscopic spine surgery, more so in case of those with symptoms related to nerve compression.
What are the benefits of endoscopic spine surgery?
Smallest possible incisions and hyper-targeting of the surgical site causes less trauma to the adjacent structures like skin, muscle, and soft tissues and most ESS procedures take about one hour to perform. This has many benefits like:
- Since ESS can be done under local anaesthesia in most cases, it does not require hospitalization, allowing a person to be back on their feet a few hours following post-operative recovery.
- The risk of post-surgical infections is lesser as compared to open or other forms of spine surgery.
- The small size of incision causes minimal blood loss and there is the least scarring.
- A person’s pain experience is minimal during and after the procedure.
- Reduced trauma to adjacent tissue leads to faster recovery and quicker return to normal life.

Is endoscopic spine surgery safe? What are the risks?
Just like any other surgical procedure, ESS is not devoid of risks and there are general risks and procedure-specific risks. Some of the general risks of spine surgery include the risk of:
- Adverse reactions to anaesthesia
- Postoperative pneumonia
- Formation of blood clots in the legs or deep vein thrombosis that may travel to the lungs causing pulmonary embolus
- Infection at the surgical site, a fluid leak from the incision should be carefully observed for any increase. Fever or pain that gets worse, trouble breathing, or a severe headache call for an emergency consult with the doctor.
- Excessive blood loss during surgery.
The procedure-specific risks of ESS include the risk of:
- Injury to the adjacent structure like nerves or spinal cord that may lead to pain or even paralysis in some cases.
- Breaking or dislodging of the instrument
- Irritation of the surrounding tissues
- Excess pain
- Sometimes a planned ESS may need to get converted to a full open technique or may require revision after the first surgery.
Recovery after endoscopic spine surgery, how long does it take?
A person could expect a long recovery, as much as a year in some cases until a few years ago. However, with the advancements in minimally invasive surgery techniques, especially endoscopic spine surgery, the overall recovery period has been reduced to a few days or less with a few small scars at the site of the incision.
Since the majority of the ESS procedures are done on an outpatient basis, a person can expect to go home the same day. Depending on the overall health, after the procedure a person will be made to stay for a couple of hours or a day or two for observation. While there may be some amount of pain after the surgery, it can be relieved with pain medications prescribed by the treating surgeon.
A person can resume a normal diet as soon as you one can.
The spine surgeon advices instructions about the usage of the back after the surgery. Some of these maybe
- Limit lifting or bending till full recovery.
- Wear a back brace for some time after the procedure.
- Physical therapy may be required after the surgery to help strengthen muscles around the spine.
The overall recovery time of a person may vary depending on the type of surgery and general health. However, one can resume normal activities within a few weeks.
For a quicker and safer recovery and successful surgery, one should ensure adherence to the spine surgeon’s instructions about treatment and follow-up appointments.
How should one choose a facility for endoscopic spine surgery?
Most important nerves of the body’s functioning originate from the spine, making it a very vulnerable site for open surgical procedures. One of the main objectives of the endoscopic spine surgery is to avoid collateral damage to the adjacent tissues. This objective can be achieved by a precise diagnosis, sophisticated equipment, and spine surgical expertise which is usually not available collectively at most of the healthcare settings. Hence the treatment facility is available only at a few select super-speciality hospitals of India.
The decision to have spine surgery is an important one that needs to be seriously taken collectively by the affected person, family and the spine surgeon. Finding the right facility and surgeon to perform endoscopic spine surgery is paramount in a successful surgery and also to ensure that the person is comfortable with the decision to have surgery.
Some of the reasons for the rarity of spine surgery experts specializing in endoscopic spine surgery are:
- Due to the complexity of the technique, the learning curve is steep.
- There are limited training institutes and facilities and most of the existing ones are of recent origin.
- The equipment is expensive.
- Mastering the technique requires exceptional three-dimensional skills.
Conclusion:
Endoscopic spine surgery is a highly specialized technique that should not be confused with other types of minimally invasive or laser spine surgeries. The endoscopic spine surgery is performed using tubular retractors and the endoscope with a high definition camera, making it the least invasive of all surgical procedures of the spine. In the hands of a highly skilled and experienced spine surgeon, the potential benefits of this extremely advanced version of minimally invasive surgery promises relief to many persons living with chronic back and neck pain.
ESS has many potential benefits, including:
- Negligible blood loss
- Less postoperative discomfort and pain
- Faster recovery and quicker healing
Generally, people leading an active, healthy lifestyle are the most suitable candidates for endoscopic spine surgery. However, a spine surgeon should be consulted for an opinion on suitability to undergo the procedure even in people who are not in the best of health.
Despite its benefits, ESS may not be a suitable option for all conditions of the spine such as scoliosis, spinal instability, cancer, or trauma where a traditional open or minimally invasive spine surgery may be a better option.
For more information please request a call-back and our health experts will get in touch with you.
References:
- American Association of Neurological Surgeons. Minimally Invasive Spine Surgery. Available at: https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Minimally-Invasive-Spine-SurgeryAccessed on October 11, 2019
- Johns Hopkins. Minimally Invasive Spine Surgery. Available at: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/minimally-invasive-spine-surgery. Accessed on October 11, 2019
- International Journal of Spine Diseases. Full Endoscopic Spinal Surgery Techniques: Advancements, Indications, and Outcomes. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4480053/. Accessed on October 11, 2019
- Journal of Korean Neurosurgical Society. Endoscopic Spine Surgery. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5594628/. Accessed on October 11, 2019








 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





