How to treat Parkinson’s Disease using Deep brain stimulation?
Parkinson’s disease is a movement disorder. It is marked by slow progressive damage to the brain cells. This age related disease is largely presented in people when they are above 50 years of age. However, there are cases where the symptoms are visible as early as in age group under 40.
How to treat Parkinson’s disease?
Parkinson’s disease is treated symptomatically, there is no total cure for this disease. When diagnosed early, doctors treat the disease to slow the onset of motor (movement) symptoms. Motor symptoms may include tremors, rigidity, postural instability, bradykinesia (slow and difficult movement), and parkinsonian gait (shuffling walk; mid-stride freeze with forward fall).
Medications aim to increase the levels of dopamine and improve dopamine related functions. This treatment is effective for patients in earlier stages of Parkinson’s disease. These patients are regularly monitored for worsening of the motor symptoms. For some patients with advanced Parkinson’s disease, surgical therapy may be an option.
Many patients respond well to treatments and live a normal life with little to moderate disability. While others may not respond well, resulting in severe disability. Here, we shall discuss the advances in the medical sciences that is enabling Parkinson’s disease patients to enjoy an improved quality of life.
Other than surgical and medical therapies, there are some restorative therapies that might help. However, these therapies are not standardized for clinical use, they are still in experimental stage and pending FDA approval for being used as standard care for patients.
When should one consider surgical therapy?
Parkinsonian symptoms worsen as the disease progresses. Classic antiparkinsonian medicines help maintain a better quality of life. However, long-term adverse events such as dyskinesias cause troublesome writhing and jumping of the body.
In addition, “on-off” fluctuations are observed along with the beneficial effects of antiparkinsonian medicines. The medication seems to work at times and at other times normal movement becomes very difficult. These shortcomings of medicines lead to poorer quality of life as years roll on. This is when surgical treatment should be considered.
What are the different types of surgery for Parkinson’s disease?
Surgical therapy for Parkinson’s disease include ablative (or brain lesioning) procedures and deep brain stimulation (DBS). Ablative or brain lesioning procedures are the first surgical procedures developed for Parkinson’s disease.
Ablative brain surgery:
Ablative brain surgery is also known as therapeutic brain lesioning. The process involves precisely controlled destruction of a small region of brain tissue, with help of a heat probe. This enables to improve symptoms that are produced from these brain tissues. Thalamotomy and pallidotomy are some ablative or brain lesioning procedures.
In general, it is not safe to perform lesioning on both sides of the brain. This surgical method fell out in 1980s for its mixed results. However, advances in imaging technology enables improved results in treating advanced Parkinson’s disease. However, DBS surgery has largely replaced the ablative surgeries. We at Yashoda Hospitals continue to perform ablative surgeries only for patients who choose it over DBS surgery.
DBS surgery:
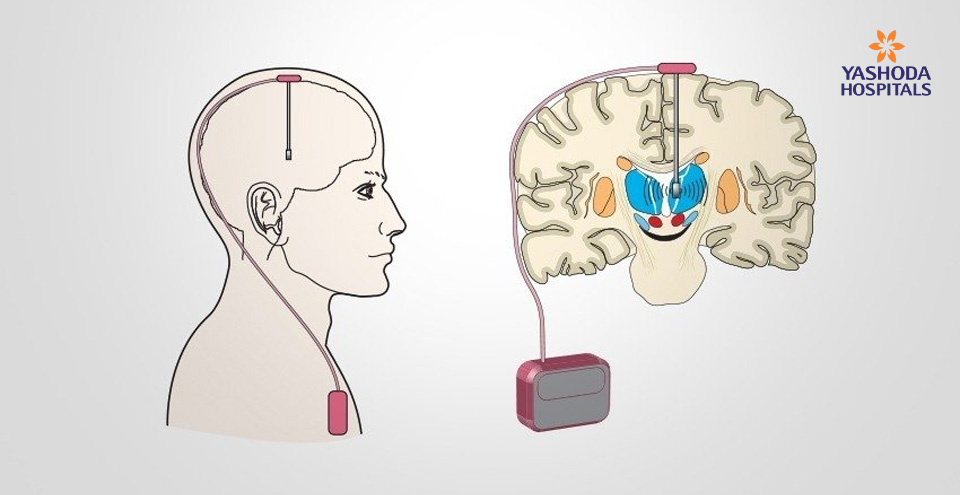
Deep brain stimulation is the surgical method which involves placing a thin metal electrode in several possible brain targets. Electrical stimulation of target brain cells improve relevant Parkinsonian symptoms.
In DBS surgery, a thin metal electrode of a size of ‘thick noodles’, is placed in the areas of brain that doctors intend to stimulate. These electrodes are then connected to a computerized pulse generator, which is implanted under the skin in the chest. Altogether, this stimulator system is completely internal. There are no wires extending out of the skin which needs daily care.
Maximal relief from symptoms is achieved by reversible alteration of abnormal functioning of the brain tissue in the region using electrical stimulation. Electrical stimulation does not destroy the brain tissues unlike ablative surgery.
DBS is most often recommended at Yashoda Hospitals for movement disorders. Though, DBS is a new advance in the treatment of Parkinson’s disease and other movement disorders. This complicated therapy demands considerable patience and time before its beneficial effects are optimized and enjoyed.
How to target brain cells for DBS?
There are small clusters of nerve cells that influence and control voluntary body movement. Relief from Parkinsonian symptoms is achieved by targeting these nerve cell clusters:
- Internal segment of the globus pallidus (GPi)
- Subthalamic nucleus (STN)
- Subdivision of the thalamus referred to as Vim (ventro-intermediate nucleus)
- Pedunculopontine nucleus (PPN)
These are the four possible target sites in the brain that may be chosen for placing the electrodes. However, only 3 of these targets are now approved by the U.S. Food and Drug Administration.
- Thalamic (Vim) stimulation: DBS of subdivision of thalamus is effective for tremors but not for other symptoms of Parkinson’s disease.
- Globus pallidus (GPi) Stimulation: DBS stimulation of globus pallidus treats tremors along with other Parkinsonian symptoms such as rigidity, bradykinesia, gait problems and dyskinesias.
- Subthalamic nucleus(STN) Stimulation: DBS stimulation of globus pallidus treats tremors along with other Parkinsonian symptoms such as rigidity, bradykinesia, gait problems and dyskinesias.
Pedunculopontine nucleus (PPN), is an investigational target. This DBS stimulation is considered to be effective for patients with gait freezing. This target DBS requires further studies to be a part of standard care. Most patients of Parkinson’s disease benefit from DBS of Globus pallidus and subthalamic nucleus as they improve broader range of symptoms.
How does DBS work?
Deep brain stimulation of GPi or STN was studied in the late 1980’s and early 1990’s. Scientists found that dopamine forming cells in the brain progressively degenerate leading to excessive activity and abnormal pacing of activity at GPi and STN. This causes serious movement symptoms in Parkinsonian patients.
DBS at GPi and STN is considered to compensate for this major secondary effects of dopamine loss, rather than directly affecting dopamine producing cells or altering brain dopamine levels. DBS enables pacing of these nuclei so that the electrical pulses generated by these nuclei are constant and steady.
How to perform the surgery?
A brain imaging study (MRI) is done few days before the actual surgery for planning. Commonly, DBS surgery is performed with local anesthesia or occasional sedation. The patient remains awake during the process.
Stereotactic surgery:
Stereotaxy is surgical method used to approach deep brain targets through a small skull opening.
The patient is prepared for the surgery, the skin is anesthetized with a local anesthetic. After which, a rigid frame is attached to the patient’s head. With the frame in place, a CT is obtained to view images of the brain and the frame. This enables the neurosurgeons to calculate the position the brain target (GPi / STN). Accordingly, doctors guide the instruments to the target areas with minimal chances of brain trauma during the procedure. The patient is then taken to the operating room.
The stereotactic frame is then fixed to the operating table. A Foley catheter is placed in the bladder. A patch of hair on head is shaved and scalp is washed. The scalp is then anesthetized to complete numbness. A surgical incision is performed behind the hairline to create a small opening (1.5 centimeters, size of a coin) in the skull.
Brain mapping:
To achieve high precision with successful outcomes, brain mapping is essential for DBS surgery. Brain mapping (micro electrode recording), involves recording brain cell activity of the DBS target region. The procedure may also be used to fine tune (fine adjustments of 1 to 2 mm) the intended brain targets, in case the initial target is not exactly right.
The time taken to map the brain signals may vary from 30 minutes to 2 hours for each side of the brain. The procedure by itself does not cause any sensations for the patient, but the patient should be silent, calm and cooperative. The procedure cannot be performed if the patient is not cooperative.
Electrical signals from the brain are played on a audio recorder. The readings are discussed and interpreted by the expert team of neurologists. Once the team is satisfied with the recording, macro stimulation is performed at the selected target sites to test for beneficial effects and side effects. Throughout the surgery, the neurosurgeons and neurologists evaluate the neurological status of the patient which include improvement in the motor function, vision, speech, strength and more.
Testing at high intensity stimulation:
Doctors deliberately test the effects of stimulation at an intensity higher than normal, in order to ascertain the possible stimulation-induced side effects. These side effects may include flashing lights, difficulty speaking, tingling in the arm or leg, or a pulling sensation in the tongue or face. These sensations are experienced as strange but they are not painful. This test is necessary to confirm that the stimulation intensity needed to produce such effects is higher than that normally intended for long-term use of the device.
Once the neurosurgeons insert the permanent DBS electrode and test it successfully, the patient is then sedated intravenously. Then the electrode is anchored to the skull and scalp incision is closed with the sutures. Finally, the stereotactic head frame is removed.
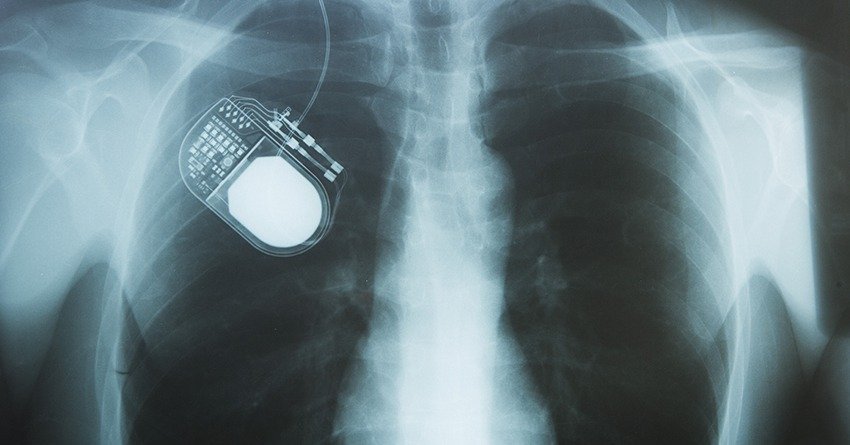
Implanting the pulse generator:
The pulse generator is surgically implanted in the chest. Then tunneling of the connector wire between the brain electrode and the pulse generator unit is performed. For this procedure, the patient receives general anesthesia and it takes about an hour for surgeons to complete the implantation and tunneling.
Would both sides of the brain be done at once, or only one side?
The symptoms of Parkinson’s disease may be elicited due to poor brain functioning from both the sides. DBS when performed on one side shows improved symptoms on the opposite side of the body. Usually, patients receive DBS on both sides of the brains for maximal benefits.
Previously, each side of the brain were stimulated separately months apart. However, the surgery is now performed more regularly these days and “simultaneous bilateral” procedures, or implantation of both leads is now performed in a single surgery.
Neurosurgeons perform DBS on the brain side opposite to the affected body side first. Once, this is done, he performs DBS on the other side after a consent from both the patient and the anesthesiologist. In cases where the surgery may prolong longer than intended and in elderly patients, DBS may be staged several months apart.
What are the benefits of DBS surgery?
DBS surgery improves the “on-off” effect of the medication. DBS enables movement even in the off-medication state similar to the movement in the on-medication state. Also, it improves medication-induced dyskinesias, directly or by enabling a reduction in medicine doses. Therefore, Parkinson’s patients who experience states of mobility and states of immobility (“on-off” states) benefit the most out of DBS surgery.
DBS smooths the fluctuations in the states of mobility. Alongside, DBS also improves any symptoms that are improved by antiparkinsonian medicines (slowness, stiffness, tremor, gait disorder). Any symptoms that do not improve with antiparkinsonian medicines does not significantly improve with DBS surgery. DBS surgery may only reduce but not eliminate the use of medications. In simple terms, DBS surgery only improves the symptoms but does not in any which way alter the course of disease progression.
What are the risks or complications of DBS surgery?
DBS surgery is a major brain surgery which is associated with risks that include:
- Temporary swelling near the electrodes
- Bleeding and stroke
- Infection
Bleeding in the brain and stroke: Bleeding in the brain and a potential risk of a stroke is the serious possibility during or couple of hours post surgery. The risk of bleeding and stroke varies based on the individual and health status. However, the average risk of DBS associated bleeding and stroke is only 2%. The effects of stroke may be mild to severe and the patient may recover in a few weeks or months. In other cases, stroke can lead to permanent weakness, cognitive impairment or death.
Infection: Infection is another serious risk associated with DBS surgery. However, infection is usually not life threatening. Only 4 in 100 cases experience DBS related infections. If infection does occur, it may require removal of entire DBS system. In most cases, a new DBS system can be re-implanted when the infection is eradicated.
Temporary swelling: In the first few days after surgery, it is normal to have some temporary swelling of the brain tissue around the electrode. This may produce no symptoms, but it can produce mild disorientation, sleepiness, or personality change that lasts for up to 1-2 weeks.
Hardware damage: The device may break or erode through the skin with normal usage. The patient needs a replacement device.
What tests are needed prior to surgery?
Before a DBS surgery can be scheduled, the patient needs to undergo brain imaging tests (either MRI or CT) to determine if there are any problems in the brain that would pose excessive risk for surgery. If brain imaging is already done, it should not be older than a year.
Patient will then undergo formal neurological exam in off-medication condition and in test dose of medication. Once the neurologist confirms the results, the patient undergoes blood tests and visits anesthesiologist a week before surgery. For any patient with a question of cognitive dysfunction, a formal neuropsychological evaluation may also be requested.
How to prepare patients for surgery?
A week before: Patient planning for DBS surgery should stop medicines that increase the risk of bleeding 7 days prior to surgery. Talk to your neurologist and neurosurgeon about all the medications you take.
Evening before surgery: Patient should wash head, neck, and chest with soap in the shower.
Morning of surgery: The patient should not take their antiparkinsonian medications. If the patient has other health conditions such as blood pressure, the patient should take any medications they normally take. The patient shall inform the surgeon if they develop a cold, cough, or any type of infection in the days prior to the surgery. The patient should be well hydrated prior to surgery (drink a lot of non-alcoholic, non-caffeinated drinks).
What type of follow-up is needed after surgery? Who will program the DBS unit?
Post surgery, patients are monitored in the hospital for 1 week. Some patients may experience temporary disorientation or sleepiness for a few days. This is due to temporary swelling in the DBS targets around the electrode.
The initial programming is done at Yashoda Hospitals usually at the one-week postoperative visit. In case of temporary swelling, the programming is deferred until the mental state returns to normal completely.
After discharge, patients return to hospital 1 or 2 weeks later for suture removal and a follow-up with neurosurgeon and neurologist. For subsequent programming needs after the initial stimulator activation, the patient is welcome for continued support by our team.
Replacement of pulse generator, is an outpatient procedure that takes about 60 minutes.
The pulse generator may need to be replaced after 4-6 years, depending on the exact settings of the device. The rechargeable pulse generators may be used which works longer and needs replacement only after around 10 years.
How long does it take before the full benefit of DBS is apparent?
The benefits of DBS are apparent in a few hours in some cases, while in others it is delayed for a few days. The reasons for this duration is not clearly understood. Also, certain symptoms respond quickly than the others. For complete benefits from DBS, the patient may need a change in medicines and multiple programming sessions. Thus it is usually a few months after surgery before the final degree of benefit is actually realized.
Can patients control the DBS device themselves?
Post surgery, the patient receives a hand-held battery-operated remote to switch the device on or off, and to check battery life. But for Parkinson’s disease patients, the device remains on all the time. The patient is allowed some controls on stimulation levels as per the limits set by the doctor.
Are there any restrictions on a person’s activity after a DBS system is implanted?
The DBS system does not affect the normal physical activity. The patient is advised to resume all normal activities, exercises after the incisions are completely healed (2-3 weeks). The DBS system does not pose risk around security devices (such as those in airports or stores), although in rare cases they may activate the on-off switch, thus turning off a DBS system that had been on. It may take a while for the patient to realize the loss of benefit (minutes or hours). Therefore, the patient is advised to remain vigilant and use the patient control unit (remote) to reactivate the DBS system, when traveling extensively and away from home.
Can I have an MRI scan after DBS?
At Yashoda Hospitals, we have developed a specialized, low-energy protocol for brain MRI, allowing us to perform postoperative brain MRI safely. Patients with DBS implant are advised to avoid most of the MRI exams so as to prevent heating of the brain electrode. If the patient is undergoing spine or chest MRI, the DBS device should be shut down. The MRI should be done by the experienced physician within the MRI restrictions in DBS implanted patient.
Summary
Neuroscience is growing and evolving. Parkinson’s disease is now treatable with more medical and surgical treatment options than ever before. Deep brain stimulation surgery is one such innovation that improves Parkinson’s symptoms. DBS offers benefits in patients with moderate disability from Parkinson’s disease who still respond to medications and who are cognitively intact. Patients who experience “on-off medication” states are good candidates for DBS surgery. Patients with troublesome dyskinesias also equally benefit from the surgery. The major risk is a less than an 2% risk of stroke, due to bleeding in the brain. DBS is a relatively complex therapy requiring regular neurological follow-up. It reduces, but does not eliminate, symptoms of Parkinson’s disease. The time to consider DBS surgery is when quality of life is no longer acceptable on optimal medical therapy as administered by a movement disorders neurologist.
About Author –
Dr. Anandh Balasubramaniam, Senior consultant and HOD, Neurosurgery, Yashoda Hospitals, is a renowned neurosurgeon in Hyderabad. His expertise include neuro-oncology, intraoperative MRI and image guided neurosurgeries, endoscopic surgeries, endoscopic minimally invasive surgeries, deep brain stimulation and functional neurosurgeries.






 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





