Trans-femoral-brachial approach for the percutaneous angioplasty of eccentric stenosis

A combined approach for Right innominate artery PTA
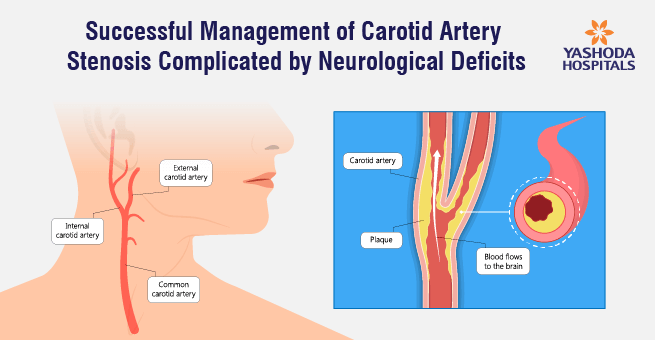
Right brachiocephalic stenosis is usually discrete short segment lesions but they most difficult to intervene for certain reasons. Their takeoff from the arch of aorta and eccentricity of the Stenotic lesion may pose problems while intervention. Also, there is a controversy about the use of distal protection device during angioplasty.
There are many methods described for its interventions but trans-brachial access is easier to tackle difficulties those may arise with the transfemoral approach. We describe a case of right brachial-cephalic high-grade Stenosis, which was difficult to access by trans-femoral approach but trans-brachial access solved our problem and we could deploy the stent across the lesion with ease.
Combined Antegrade Diagnostic and Retrograde Interventional Approach for the Management of Right Brachiocephalic Artery Stenosis
Introduction:
The inability to cross guide wire is one of the main reasons for failure in percutaneous stenting of the ostio-proximal stenosis of right brachiocephalic artery. The difficulty is usually a tortuous aortic arch or an unfavorable supra-aortic takeoff. Several techniques are described to overcome this problem. In this case report, we describe a combined technique that we have found to be quite useful in patients who have an unfavorable arch anatomy and eccentric lesion, which was difficult to cross. We have used a specific case as an example to illustrate this technique.
Learning Objectives:
Right brachio-cephalic artery stenoses are difficult to access due to the eccentricity of the lesion and unusual takeoff from the arch of the aorta. Combined trans-femoral and transbrachial approach can be an easy way to tackle these difficulties.
Case Report:
A 55 years old male, heavy smoker and hypertensive presented with weakness of left upper and lower limb since 2 days with aphasia. The patient had normal vital signs. Upon admission, the patient was subjected to the computed tomography of the brain, which showed right thalamic infarct. Hence patient was started with aspirin 150 mg, clopidogrel 75 mg, enoxaparin 60 mg.
The patient recovered of his symptoms next day and computed angiography of supra-aortic vessels revealed critical stenosis of the proximal segment of the right brachiocephalic artery, normal left carotid, and subclavian arteries. After consultation with Neuro physician and radiologist percutaneous transluminal angioplasty was planned after 2 weeks.
The right femoral artery was cannulated using 6Fr. sheath and 6 Fr. right coronary guide catheter to engage the right innominate artery. There was difficulty in crossing the stenosis, as it was eccentric lesion [Figure 1A]. After some efforts, whisper extra support guide wire could cross the lesion and be pre-dilated using 5.0 x 15 mm balloon [Figure 1B]. We tried exchanging with 8 Fr. Sheath but it could not be negotiated up to right brachiocephalic artery.
Hence right brachial artery was cannulated and 0.035 wire was crossed easily retrograde into the descending aorta [Figure 1C]. Through the trans-femoral approach, the right coronary diagnostic catheter was used for the visualization of the stent across the lesion [Figure 1D]. Also, the radioopaque marker [scalpel handle] was placed externally across the midpoint of the lesion and cath lab table was fixed. The 10 X 37 mm Scuba balloon-expandable stent was deployed across the ostio-proximal segment of right innominate artery [Figure 1E].
Check angiography revealed the good expansion of the stent and normal flow across the carotid-vertebral and subclavian artery [Figure 1F]. The patient had no neurological deficit and discharged on 2nd-day post procedure with the advice of optimal medical management in the form of dual anti-platelet agents [aspirin and clopidogrel], ACE inhibitor, beta-blocker, a high-intensity statin.
Discussion:
Earlier in 1950 to 1970, there are several reports and case series of management of high-grade stenosis of aortic arch vessels with surgical repairs with high morbidity and mortality rates. Later in 1970s percutaneous modalities of treatment emerged to manage peripheral vessels like renal, carotids, mesenteric vessels etc
In In(1) Since then, percutaneous angioplasty with a stent is rapidly becoming a common method of treatment for right brachio-cephalic stenosis. As interventionists have gained wide experience with this procedure, several technical modifications of the technique for gaining access to the involved innominate arteries have been described.
In India, the most common etiology is atherosclerosis and Takayasu’s aortoarteritis. Symptoms range from ischemia of the right upper extremity to the anterior or posterior cerebral circulation or a combination of upper extremity and diffuse neurological symptoms(2).
In three case series of percutaneous angioplasty of right innominate artery stenosis, the procedural success rate of varied from 96.4% to 88%.(3–5) In all the case series, the indications for endovascular treatment were as follows: neurologic symptoms, upper limb claudication or digital embolization, asymptomatic patients with the multi-vessel disease with or without subclavian steal syndrome(3).
In our case, the technical challenge was primarily crossing the lesion and maintaining support of the sheath secondary to anatomical difficulties imposed by a very high-grade stenosis. In the case series by Paukovits et al, 5.6% of innominate artery lesions could not be crossed via a transfemoral approach. Hence, they performed right brachial artery cannulation to access sight innominate stenosis and to deploy stent as in our case(3).
Peterson et al in their single-center experience of aortic arch vessel stenting performed 8 cases of innominate artery stenting. They have used combined approaches for the angioplasty of innominate artery stenting. In one of their case, they did retrograde stenting via brachial artery puncture without using neuro-protection device due to technical difficulty as in our case (1).
Conclusion:
In our case, there was an eccentric lesion, which was difficult to cross hence; we adopted a combined approach for the intervention of the right brachiocephalic artery stenosis. The success rate of right innominate artery angioplasty has increased due to combined approach, availability of new, lower profile balloons and stents and experience of interventionists. Percutaneous angioplasty of right innominate artery using stent improves long-term outcome.
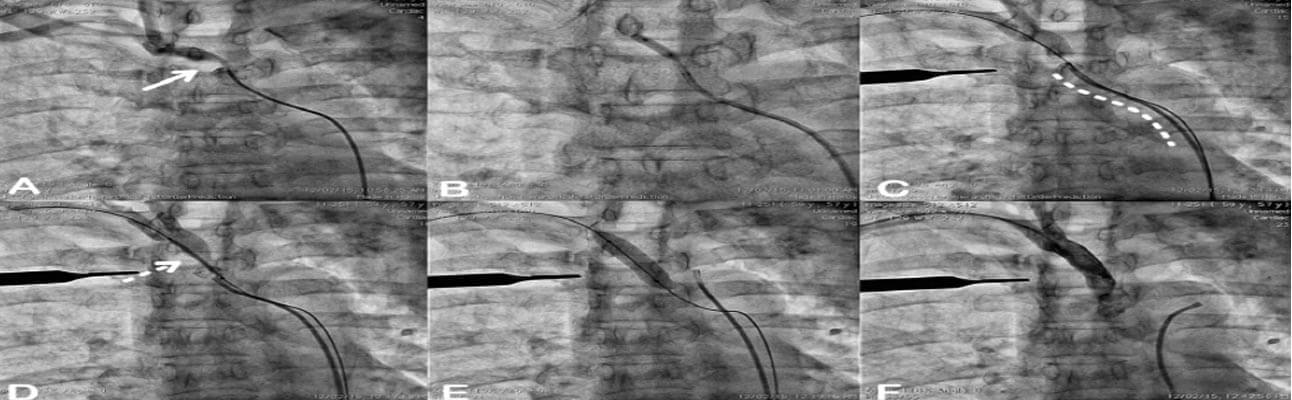
Figure Legend:
Step wise demonstration of peripheral percutaneous angioplasty of right brachio-cephalic artery stenosis which was eccentric [Solid arrow, Panel A] and unfavorable supraaortic takeoff [Dotted curvilinear line, Panel C] from the aortic arch. Initially, the transfemoral approach was used and could cross with coronary 0.014’ whisper extra support guide wire using a 6Fr right coronary guide catheter [Panel B]. The lesion was dilated using 5.0 x 15 mm balloon [Panel B]. For the deployment of a stent, we could not negotiate a larger 8 fr. Guide catheter/delivery sheath [Not Shown]. The transbrachial approach used to deploy 10 x 37 mm balloonexpandable stent across the lesion [Dashed arrow, Panel D] under angiographic guidance from trans-femoral right coronary diagnostic catheter [Panel E] and externally placed scalpel handle across the lesion as a radiopaque marker [Panel C-F]. Final check angiography showed no residual stenosis with the brisk flow [Panel F].
Bibliography:
- Peterson BG, Resnick SA, Morasch MD, Hassoun HT, Eskandari MK. Aortic arch vessel stenting: a single-center experience using cerebral protection. Arch Surg 2006;141(June):560-563-564.
- Ryer EJ, Oderich GS. Innominate Artery Stenting Under Embolic Protection. J Endovasc Ther 2010;17:652-6.
- Paukovits TM, Lukács L, Bérczi V, et al. Percutaneous endovascular treatment of innominate artery lesions: A single-centre experience on 77 lesions. Eur J Vasc Endovasc Surg 2010;40:35-43
- van Hattum ES, de Vries JPPM, Lalezari F, et al. Angioplasty with or without Stent Placement in the Brachiocephalic Artery: Feasible and Durable? A Retrospective Cohort Study. J Vasc Interv Radiol 2007;18(9):1088-93.
- Hüttl K, Nemes B, Simonffy Á, et al. Angioplasty of the innominate artery in 89 patients: Experience over 19 years. Cardiovasc Intervent Radiol 2002;25(2):109-14.
About Author –
Dr. Pankaj Vinod Jariwala, Consultant Interventional Cardiologist, Yashoda Hospitals – Hyderabad
MD, DNB, DNB, MNAMS, FICPS, FACC.
Fellowship in Interventional Cardiology [ICPS, Paris, France]He has performed 5000+ percutaneous trans-luminal coronary Angioplasty & 10,000+ Coronary Angiograms and treated 500+ structural heart diseases (including congenital) with Percutaneous Balloon Mitral Valvuloplasty [PBMV] and other pediatric & adult cardiac interventions.









 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More