TAVR for 81-year old NYHA class III patient with aortic stenosis
An 81-year-old African male was admitted with complaints of the progressive shortness of breath (NYHA class III) on exertion for 3 months. He had also complained of paroxysmal nocturnal dyspnea along with swelling of the lower limbs for the past month. He had undergone PTCA to the right coronary artery in 1999. He consulted a local cardiologist who performed echocardiography that revealed the presence of severe left ventricular dysfunction with severe calcific aortic stenosis.
Since his STS score was high, he was recommended trans-catheter aortic valve replacement [TAVR]. He travelled to India to get advanced interventional therapy.
His vital parameters recorded were: pulse rate of 68/minute and blood pressure of 110/70 mm Hg. Clinical examination revealed pitting bilateral pedal edema, and on auscultation, there was ejection systolic murmur grade III/VI radiating to both carotids. After admission, we performed routine laboratory investigations which was normal except for serum creatinine of 1.3.
Electrocardiography demonstrated sinus rhythm and left ventricular hypertrophy with strain pattern. Echocardiography showed dilated chambers, global hypokinesia of left ventricle and severe left ventricular dysfunction [EF- 30%] with grade III diastolic dysfunction. Doppler interrogation of aortic valve revealed high gradient [peak gradient – 74 mm Hg and mean gradient – 37 mm Hg], AVA by continuity equation – 0.9 cm2. There were specks of calcium over the aortic cusps. Color flow mapping of the mitral valve demonstrated moderate mitral regurgitation. There was mild dilatation of right ventricle and mild tricuspid regurgitation with right ventricular systolic pressure of 50 mm Hg.
He was subjected to CT aortic angiography that confirmed the suitability of TAVR. All the parameters were suitable except the height of left coronary artery which was 7.9 mm. It was a bit lesser than the optimal height of 10 mm.
In view of severe renal impairment, he was adequately hydrated in consultation with nephrologist. His creatinine rose to 1.4 mg%. After 2 days, he was subjected to conventional coronary angiography to reduce the amount of contrast. CAG revealed tight stenosis of the mid segment of the LAD. Also there was significant long segment tandem stenosis of the mid-distal segments of the right coronary artery.
PTCA using three drug-eluting stents to LAD and RCA was planned in the same siting with TAVR. There is no consensus about the timing of PTCA in-patient with severe aortic stenosis who plans to undergo TAVR.
After the complete evaluation, he was subjected to percutaneous therapy that was meticulously planned with the help of Medtronic team and proctor, Dr. Gezo Fontos from Budapest, Hungary.
A team of cardiothoracic surgeons, interventional radiologists and vascular surgeons was kept on standby for the management of complications. Cardiac anesthesiologist kept him NBM from the midnight and procedure was planned for the next day after the written informed consent to the family members. All the possible complications were explained to the patient family.
The procedure was performed under general anesthesia. Left femoral artery and vein was cannulated using 6 Fr. sheaths. PTCA to the right coronary artery was done after adequate predilatation using 2.5 mm non-compliant balloon. Two overlapping resolute onyx – zotarolimus eluting stent were deployed at optimal pressure of 12 atm. Left coronary artery angiography showed haziness of the left main coronary artery. The possibility of the spontaneous coronary dissection versus calcification was suspected. Optical coherence tomography was performed, which did not show any significant stenosis with eccentric calcification. PTCA to the mid segment of the LAD was done with resolute Onyx stent. There was no residual dissection with TIMI III flow.
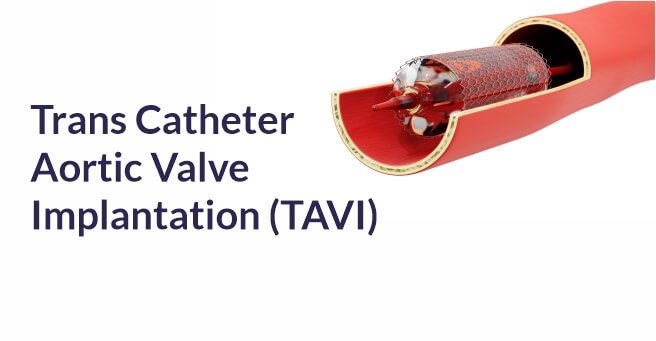
The right femoral artery was cannulated under angiographic guidance injected from the left femoral artery. The higher right femoral artery puncture was done above the femoral bifurcation, and initially, 7 Fr. sheath was inserted. Two proglides at 11 ‘o and 2 ‘o clock positions were deployed, and 18 Fr sheath was upgraded using minor surgical techniques.
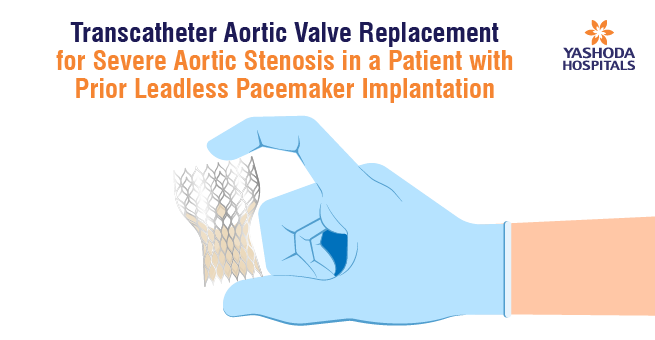
The aortic valve was crossed using AL 1 catheter and straight tip 0.035 wire. It was exchanged for the pigtail catheter that was removed after the insertion of confida wire. The peak-to-peak gradient of 60 mm Hg was measured between LV and aorta.
Initially, balloon aortic valvuloplasty using 20 mm Z-med balloon was performed under rapid pacing at 180 bpm and simultaneous aortic angiography to look for the movements of the left aortic cusp leading to obstruction of the LMCA.
29 mm Medtronic Evolute-R valve was inserted under fluoroscopic guidance and was deployed under rapid pacing at 180 bpm.
Valve position was not optimal. Hence, it was recaptured 4 times and adjusted to the optimal position. After deployment of the valve, the aortic root angiography demonstrated the moderate paravalvular leak. Hence post dilatation, it was reduced to a milder severity using a 20 mm balloon.
Femoral artery hemostasis was achieved using proglides. Patient was stable hemodynamically and shifted to CT ICCU. As parameters were stable, he was extubated next day. Patient developed bilateral moderate pleural effusion and was drained using intercostal drainage. After 2 days of observation in the ICCU, he was shifted to the floor where he was ambulated. Milder degree of the breathlessness and pedal edema was noticed. Nephrologist corrected electrolytes and escalated the dose of diuretics. A pulmonologist was also consulted, who started him on broad-spectrum antibiotics. His serum creatinine was rising with highest level reached up to 2.7 mg%, then reached nadir of 1.4 mg% before flying back home. His urinary output was normal. He was ambulatory in the ward. Few episodes of transient altered behavior and involuntary jerky movements were noticed. Neurophysician consultation was sought, who ordered EEG and CT scan brain. CT brain showed diffuse cerebral atrophy and EEG revealed abnormal electrical activity and lower serum calcium level. Anti-epileptic drug Levetiracetam (250mg) twice daily and calcium supplement settled his neurological issues. There was no hematoma of both groin and ICD sites were healing well.
He flew back to his home uneventfully, and he was in NYHA class I with mild pedal oedema.
About Author –
Dr. Pankaj Vinod Jariwala, Consultant Interventional Cardiologist, Yashoda Hospitals – Hyderabad
MD, DNB, DNB, MNAMS, FICPS, FACC.
Fellowship in Interventional Cardiology [ICPS, Paris, France]He has performed 5000+ percutaneous trans-luminal coronary Angioplasty & 10,000+ Coronary Angiograms and treated 500+ structural heart diseases (including congenital) with Percutaneous Balloon Mitral Valvuloplasty [PBMV] and other pediatric & adult cardiac interventions.










 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More