Successful Treatment of Cutaneous T-Cell Lymphoma with Total Skin Electron Beam Therapy (TSEBT)
Clinical History
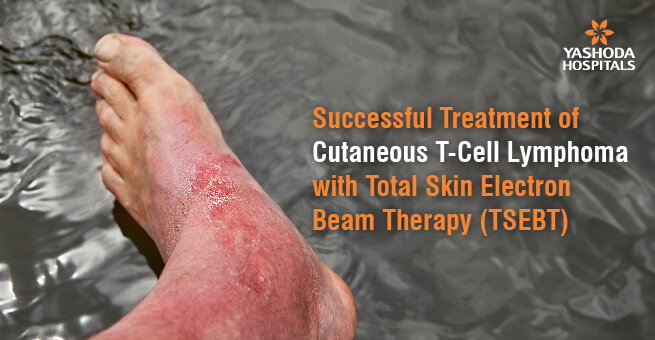
A 65-year-old male presented with a history of an itchy rash all over his body for the past six months. Initially, he tried over-the-counter creams, but his condition worsened. Subsequently, he consulted a dermatologist, who diagnosed him with Cutaneous T-cell Lymphoma (CTCL). He had a few rounds of PUVA (Psoralen plus ultraviolet A) therapy, which is a type of light therapy. However, he began to feel tired and noticed the development of skin lumps over time.
Treatment Approach
We decided to use a specialized approach known as Total Skin Electron Beam Therapy (TSET) for the patient’s treatment. In this procedure, we directed high-energy rays precisely onto the patient’s skin, and the response was notably positive, leading to substantial improvement. Only a few medical centers in India offer this advanced treatment, and the Yashoda Cancer Institute is renowned for its expertise in providing this specialized therapy. In fact, we have successfully administered TSET to ten patients, with each of them demonstrating a positive response.
Total Skin Electron Beam Therapy (TSEBT)
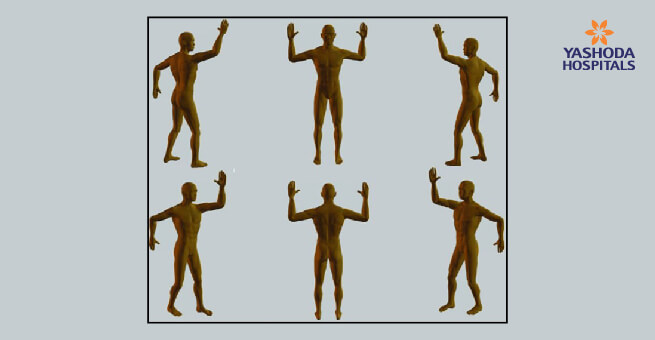
Total Skin Electron Beam Therapy (TSEBT) is a type of radiation treatment used to target specific skin cancers such as Mycosis Fungoides and Sézary Syndrome, which affect skin cells and cause patches and sores. TSEBT uses high-energy rays to damage the DNA of cancer cells, preventing their growth. During each treatment session, the patient is positioned in a specially equipped room, where the device delivers energy rays to the skin. The application of rays from multiple angles ensures uniform coverage, similar to evenly lighting a room with multiple flashlights.
Typically, treatments are administered 2-4 days a week over a span of 8-10 weeks. The patient can expect to spend approximately 30-60 minutes in the treatment room during each session. A significant portion of this time is dedicated to ensuring the patient is correctly positioned for treatment. The actual radiation procedure itself is quite brief, lasting only a few minutes. Patients undergoing treatment should avoid wearing clothing while standing in front of the radiation machine, positioned several feet away. It is important to note that the Stanford Technique is being employed for the treatment.
TSEBT is a good option for treating skin cancers that have not spread further into the body. It is particularly helpful for addressing hard-to-reach areas. Unlike other treatments, TSEBT does not harm the deeper tissues and organs. However, patients may experience skin problems, such as itchiness and redness, and, in certain instances, hair loss. During treatment, protective shields are used to protect sensitive areas such as the eyes, preventing the rays from affecting them. Additionally, periodic pauses in treatment allow the skin to recover. Prior to initiating TSEBT, a thorough assessment is conducted to ascertain its suitability for each patient, thus ensuring a personalized treatment plan that optimizes their care.
In summary, TSEBT is a highly effective radiation treatment that uses energy rays to specifically target skin cancers, effectively inhibiting their growth. This treatment is administered over the course of a few weeks, being mindful of any possible side effects and using shields to protect sensitive areas. It is important to evaluate each patient carefully and plan their treatment accordingly.

Our Experience
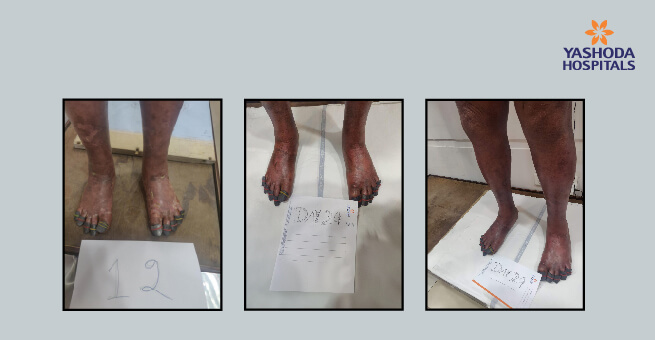
Since 2014, Yashoda Cancer Institute has handled a total of 10 cases involving TSET treatment. Six of these patients were from other countries (international), while four were from Andhra Pradesh and Telangana. While eight patients completed their treatment without any delays, typically over a nine-week period, two patients experienced a brief two-week delay due to radiation side effects, extending their treatment duration to 11 weeks. Notably, one patient had an incomplete response by the end of the treatment, prompting the administration of an additional five fractions of radiation to address residual lesions on the face. Nevertheless, all the other patients achieved complete remission and were successfully cured, with no recurrence of skin lesions observed during their follow-up.
About Author –






 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More