Recurrent Pulmonary Arteriovenous Malformation Treated with Embolization
Background
A 40 year old female patient presented with breathlessness since 8 years with recent intermittent non-pleuritic chest pain.
Clinical Examination
On examination, patient was moderately built and nourished. Vitals were pulse rate of 104/min, blood pressure 110/70 mm of Hg in right arm, respiratory rate of 30/min, Spo2 98% in room air, temperature 99 degree F. Single breath count (SBC) was 8. General examination revealed deep icterus, cardiovascular examination and chest auscultation were unremarkable and abdomen was soft. On neurological examination he was conscious, irritable, obeying commands, pupils were bilateral 2mm reacting to light, no nystagmus, normal fundus, no facial weakness and other cranial nerves examination was grossly normal. He was unable to lift his neck against gravity. Power in all 4 limbs was grade 1/5 with hypotonia and DTRs were absent with extensor plantars. Sensory level was at T5/T6 level and he had urinary retention.
Examination and Diagnosis
On examination, the patient was hemodynamically stable with a pulse rate of 90 per minute, blood pressure of 140/90 mm of Hg and oxygen saturation of 90% on finger held pulse oximeter. Examination of oral cavity showed oral telangiectasias and on auscultation of right mammary and right intra scapular area, a faint bruit was heard. Abdominal and neurological examinations were normal. Investigations showed haemoglobin of 12.1 gm/dl, packed cell volume of 56%; white blood cell count of 9,400 per cubic mm, (polymorphs 79%, lymphocytes 17%, eosinophils 2% and basophils 2%). Other biochemical parameters were within normal limits. Electrocardiogram (ECG) showed sinus tachycardia with right axis deviation and R wave in V1. Since the patient had a few episodes of epistaxis and suspicion of pulmonary embolism, the patient underwent computed Tomography Thorax and Pulmonary Angiogram. Pulmonary angiography revealed pseudoaneurysm with arteriovenous fistula arising from the right pulmonary arterial branches.
Treatment
Steal coilling was performed. Post-coiling angiogram revealed 90% exclusion of the pseudoaneurysm from the circulation. The patient improved after the procedure. The arterial blood gas analysis showed a pH of 7.430, PCO2- 38.5, PO2 – 64.7, SaO2 -87.3 and HCO3 – 25. The patient remained asymptomatic for 2 weeks following embolotherapy. Exertional dyspnoea and epistaxis due to second AVM was noted and embolotherapy was repeated. The patient now remains asymptomatic 6 months following embolotherapy.
Discussion
Osler-Weber-Rendu is an autosomal dominant disease, which may affect small portion of blood vessels at skin surface, mucosa and organs. Clinical manifestation includes nasal bleeding, skin telangiectasia, headache or bruits in cerebral AVM, chest pain or dyspnea in PAVM, malena or hematochezia in gastrointestinal mucosal telangiectasia. Diagnosis is key role for treatment of either surgical or non-surgical procedures. The surgical treatment options are embolization or silicone balloon tamponade. In general, majority of cases, embolization was performed. Also, in our case, the lesion was less than 2 cm, being an ideal candidate for embolotherapy.

Oral telangiectasias
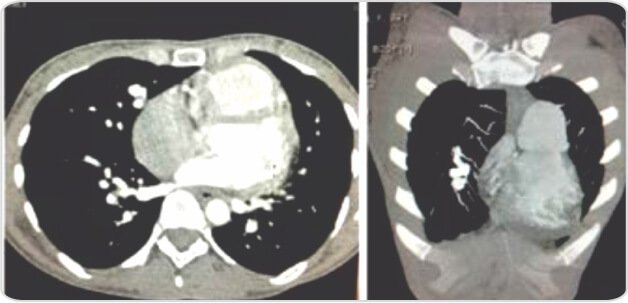
Pulmonary arteriovenous malformation

Post-coiling 90% exclusion of the pseudoaneurysm from the Circulation
About Author –
Dr. A. Guru Prakash, Consultant Interventional Cardiologist, Yashoda Hospital, Hyderabad
MD, DM (Cardiology)









 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More