Pulmonary Alveolar Microlithiasis (PAM)
Background
Pulmonary Alveolar Microlithiasis (PAM) is an ultra-rare inherited disorder of the lungs. Approximately 1000 cases of this disease have been recorded worldwide so far, with around 80 cases reported in India. In PAM, many tiny fragments (microliths) of Calcium accumulate in the lumen of the lungs’ small air sacs, progressively advancing to end-stage lung disease. There is currently no medical or gene therapy that can cure this condition. Lung transplantation is still the only option for treatment.
The case study is about our recent success in treating a 47-year-old male with advanced Pulmonary Alveolar Microlithiasis.who was treated with a Double Lung Transplant.
Diagnosis and treatment
Patient Profile:
VG is a 47 year male; a temple priest from Kakinaada, Andhra Pradesh.
He had been suffering from increasingly deteriorating shortness of breath for the previous four years and had a history of coronary artery disease (post-PTCA LAD -2010 & Stent thrombosis, PCI – 2011) and nephrolithiasis. He required oxygen initially on exertion only and then 24/7. His oxygen requirements progressively increased. At the time of the Double Lung Transplant he was on 6 – 7 liters of oxygen per minute.
Past History of the Patient:
In 2011, VG underwent coronary angioplasty with stenting of the proximal Left Anterior Descending artery. Ecosprin 75 mg, once daily, was his only antiplatelet prescription. A suitable donor became available locally on September 18, 2021. Our surgical team assessed the donor and determined that it was suitable for our patient. Both lungs were carefully harvested. A single flush of Perfadex and hypothermia were used to preserve them.
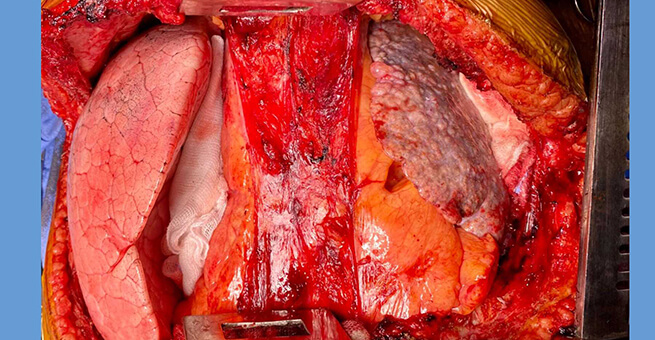
VG received Bilateral Sequential Double Lung Transplantation on Beating Heart.
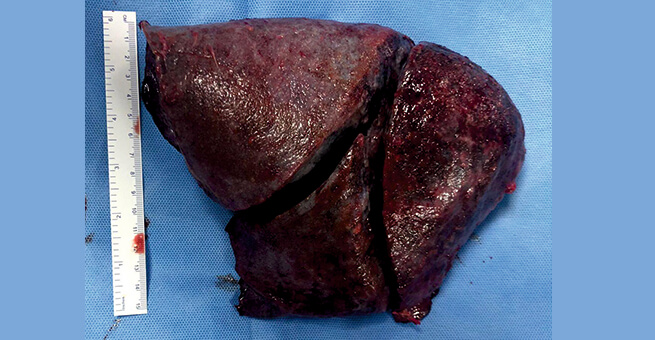
Operative Finding:
Both lungs were hard with calcific deposits. The pleura did not have any adhesions. The thoracic cavity was greatly reduced. The recipient’s Lung was too big for the Donor Lung. As a result, both Donor Lungs underwent Graft Volume Reduction (GVR). A sliver of Lung was excised from both lower lobes. Both Lungs then fitted well in the recipient thoracic cavity. The chest could be closed easily without any tamponade effect (compression of the heart). Post operation he was transferred to Transplant ICU with stable hemodynamics; on 30% FiO2 and PEEP of 10 and Oxygen Saturation of 95%.
Post Operative Course:
He had an uncomplicated post double lung transplantation convalescence. He was extubated on post-op day 3. Post extubation he was initiated into cardiopulmonary rehabilitation. He was discharged on Post op day 11.
At Discharge:
Patient was off oxygen. He was walking in our cardiopulmonary Rehab center unassisted without oxygen.
Discussion:
Pulmonary alveolar microlithiasis is a rare condition of defective phosphate transport characterised by widespread intra-alveolar accumulation of minute particles of a substance termed calcium phosphate (hydroxyapatite microliths). It is caused by mutation of the SLC34A2 gene encoding the type IIb sodium phosphate cotransporter in alveolar type II cells. These deposits eventually cause extensive damage to the alveoli and surrounding lung tissue (Interstitial Lung disease).
In most patients, PAM is discovered incidentally on radiographs performed for other purposes. The disease tends to progress slowly, often resulting in respiratory insufficiency in middle age.
The mutation of this gene leads to formation of an abnormal enzyme that transports calcium and phosphate out of type II pneumocytes.
In the Lung there are two types of cells called Pneumocytes; they are type I and type II. The microliths are formed in type II cells. Microliths also cause a reaction in the interstitial tissue that is between the cells and leads to interstitial lung fibrosis (scarring).
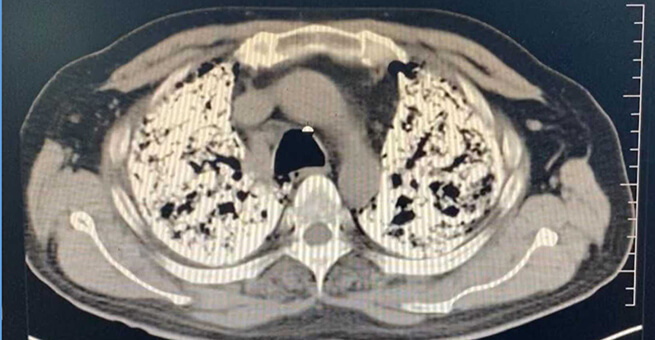
It is first seen on a plain Chest X-ray. This may be performed for some other reason like pre-employment or an annual health check up. The microliths are seen like fine sand grains (micronodular opacities )
CT scan of the chest usually confirms the diagnosis.
Biopsy may not be necessary to confirm the diagnosis.
Currently, there is no medical or gene therapy capable of removing or reducing disease progression. Systemic corticosteroids, calcium-chelating agent, diphosphonates and serial bronchopulmonary lavage have been tried. They were not effective. May be given as palliative treatment.
The definitive treatment is Sequential Bilateral Double Lung Transplantation. This is the only treatment that gives the patient a second chance to live a normal life as it has for our patient.





 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More