A Rare Case of Recurrent Sinonasal Haemangiopericytoma
Abstract
Haemangiopericytomas are a rare variety of soft tissue sarcomas. They most commonly occur in retroperitoneum, pelvic fossa and skeletal muscles. Sinonasal haemangiopericytomas are very rare and constitute less than five percent of all lesions. Very few cases have been reported in the literature. The uncertainty of the course of the disease and marked variation in the histopathological appearance of the sinonasal type of haemangiopericytomas has interested both the clinicians and pathologists. The relatively high rate of recurrence, which can occur over a span of years or sometimes decades, warrant lifelong follow up of the patient. We present such a rare case of recurrent Sinonasal Haemangiopericytoma.
Introduction
Haemangiopericytomas are rare vascular tumors arising from the pericytes investing the endothelium of the capillaries. They represent 2-3% of the soft tissue sarcomas in humans. 15-25% of them occur in head and neck region out of which 50% occur in the sinonasal region. Majority of the sinonasal HPCs are benign and have an excellent long-term prognosis. But there is a 40% chance of local recurrence and 15% chance of distant metastasis. Surgical excision with adequate margins is the standard of treatment. As local recurrence or distant spread may occur after a prolonged disease-free interval, it is essential to follow up the patients for life. We report such a rare case of haemangiopericytoma of the nose and paranasal sinuses.
Case Report
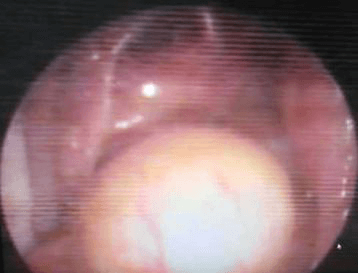
A 57-year-old female came to us in the year 2005 with bleeding from the right nostril for a duration of one month and swelling of the right upper and lower eyelids, progressive nasal obstruction and vomiting for three days. There was a history of functional endoscopic sinus surgery done outside for excision of right nasal mass in the year 1999. She had no other medical comorbidities. On examination, she was found to have widening of the dorsum of the nose. A friable mass was filling the right nasal cavity. It was bleeding on touch. Rest of the ENT examination was normal. A biopsy was taken from the lesion and the HPE findings were suggestive of inverted papilloma. In April 2005 she underwent lateral rhinotomy and excision of the mass. Intra-operatively the mass was found to be arising from the roof of the right nose extending into the right orbit. The cribriform plate was found to be dehiscent and dura was exposed in the cribriform and sphenoid area. The dehiscent area was grafted with the mucosa of the inferior turbinate. The patient was discharged in a stable condition and she was being followed up by an ENT surgeon in her hometown.
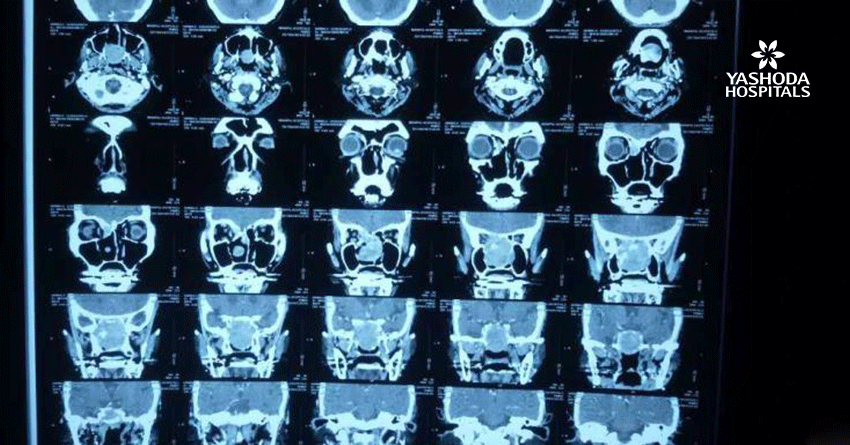
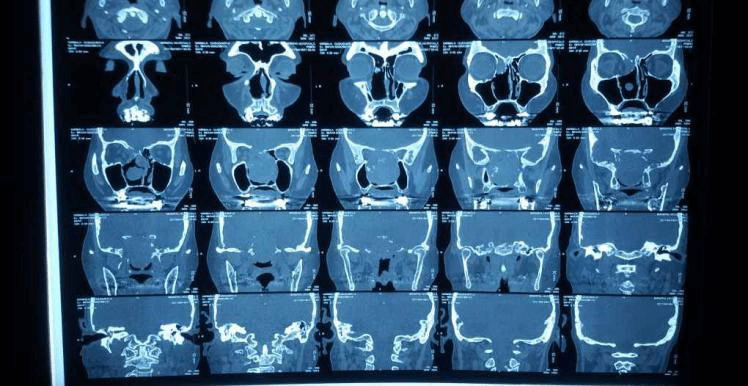
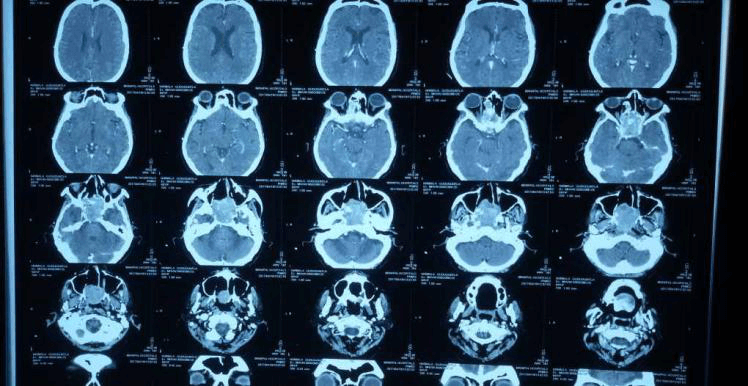
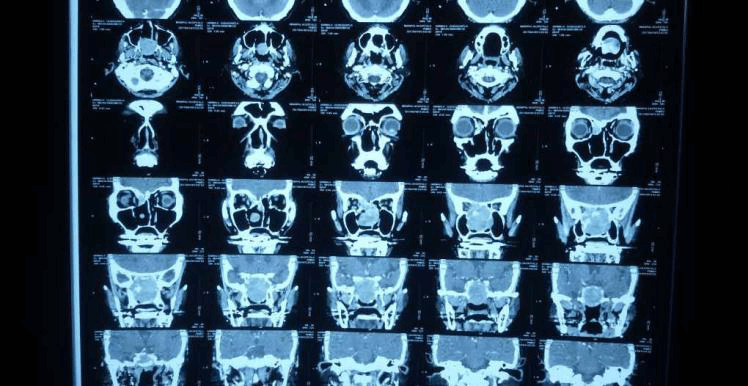
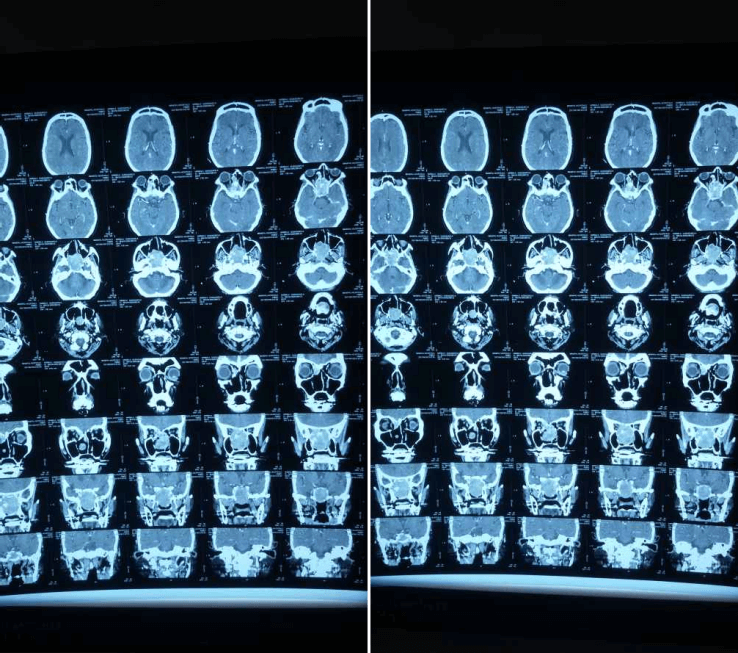
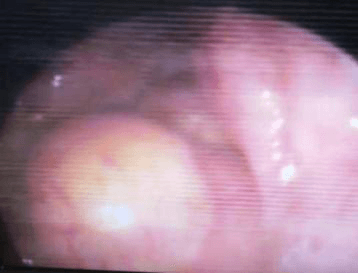
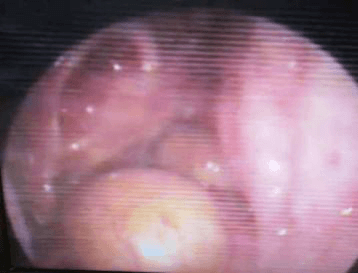
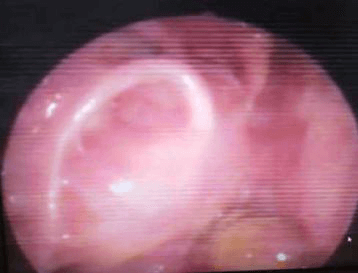
She came back to us in October 2012, complaining of gradual onset progressive right-sided nose block, purulent nasal discharge and occasional headaches of 2-year duration. There was no history of epistaxis or other ENT complaints. On examination, there was a large mass with smooth surface filling the right side of the nose, not bleeding on touch. And a gross DNS to left. MRI of the brain showed a mixed intense lesion infiltrating the base of skull sphenoid, ethmoid sinuses and part of the sella and clivus. All the routine blood and urine investigation was normal. Biopsy of the lesion suggested recurrence of inverted papilloma. She underwent endoscopic debulking of the tumor. HPE this time was suggestive of hemangiopericytoma.
She followed up, initially as OP at Yashoda Hospitals, and later with a local ENT. There was no evidence of recurrence during her visit to us two years later. Now she presented to us in the month of April with on and off right sided nose bleed for a duration of one week. DNE showed an irregular smooth surfaced vascular mass on the right. CT PNS showed soft tissue mass in the posterior part of the nasal cavity extending till the roof (cribriform plate) and filling the sphenoid sinus above and nasopharynx below. She was referred to the Department of Radiotherapy where she was advised IMRT in view of proximity to the brain and orbits.
Discussion
Haemangiopericytomas are uncommon soft tissue tumors arising from Zimmerman Pericytes located around blood vessels. They most commonly occur in pelvic fossa, thigh, retroperitoneum, skeletal muscles. Other sites are scalp, face, neck, parotid gland, orbit and rarely intraosseous, salivary glands and larynx, meninges. Sinonasal HPCs are extremely rare (less than 5% of all the lesions). Only about 200 cases have been reported in literature. HPC was first reported by Stout and Murray in 1942. The first nasal haeamangiopericytoma was reported by Stout in 1949.
It is primarily a tumor of the adults and is rare in infants and children. Peak incidence is in the sixth decade and occurs equally in males and females. Sinonasal lesions most commonly involve ethmoid and sphenoid sinuses. Majority of them are benign and have a very good prognosis with an overall ten-year survival rate of 70%. Distant metastasis occurs in about 15% of the patients whereas 7-50% chance of local recurrence has been reported. The average time of recurrence is six to seven years, but cases have been reported as long as 30 years. Distant metastasis occurs with high-grade lesions most commonly to lungs and bones, less commonly to liver and lymph nodes.
Patients generally present with nose block or epistaxis or both and sometimes with pain in the nose and headache and visual disturbances. Like other sarcomas, they can present with hypoglycemia due to secretion of IGF1 and IGF2. Clinically, a unilateral rubbery polypoidal mass of soft to firm consistency may be seen, tan or gray or whitish or vascular in appearance. Regional lymph node involvement is rare. Therefore initial presentation is frequently mistaken for nasal polyps. CT scan shows a unilateral noncalcified soft tissue shadow sometimes with bone erosion. Vascular nature can be confirmed by CECT.
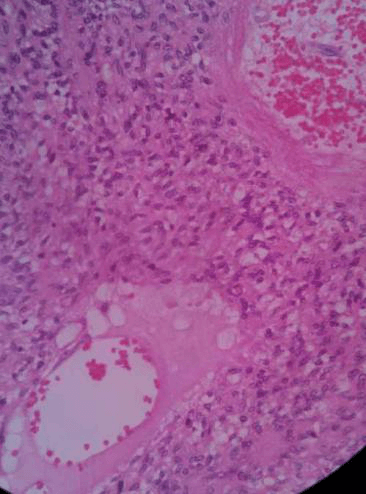
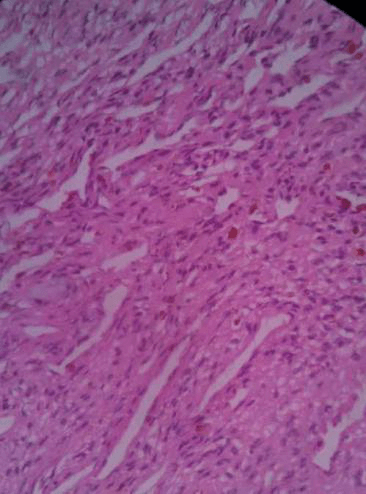
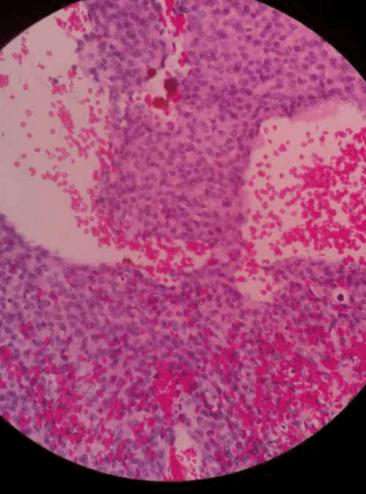
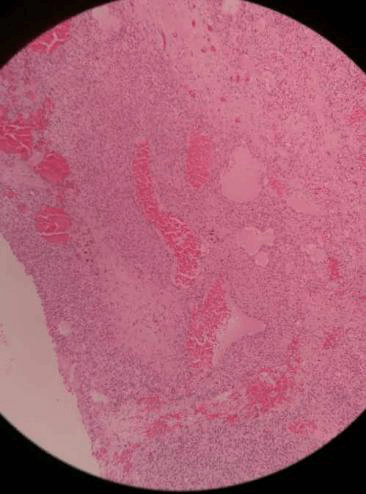
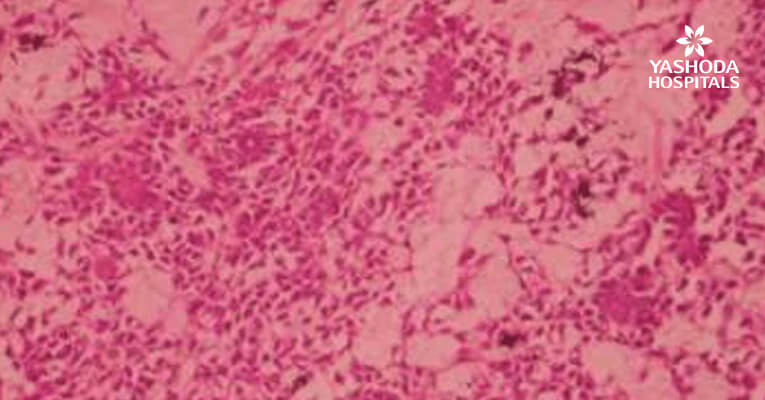
Diagnosis is by histopathological examination. HPE shows numerous staghorn type branching vascular channels with round plump or spindle-shaped cells. Tumors can be staged by histopathological features into low grade, intermediate grade and high grade based on tumor cellularity, mitotic figures, nuclear atypia, hemorrhage and necrosis. High-grade lesions have more chances of distant metastasis. Due to marked variation in the HPE appearance, HPCs can be misdiagnosed as glomus tumors, angiosarcoma, fibrous histiocytoma, lymphoma, haemangioendothelioma, and schwannoma. According to 2005 WHO classification of head and neck tumors, sinonasal HPCs can be referred to as Glomangiopericytoma due to their similarity to glomus tumors. Immunohistochemistry shows vimentin positivity invariably. Rarely they may show smooth muscle actin, desmin and S-100 positivity.
Differential diagnosis includes polyps, inverted papilloma, malignancy, fungal disease, mucocoeles, dermoid cyst, encephalocoels, meningioma, angiofibroma, chondroma, fibro-osseous lesions. Surgical excision with adequate margins is the standard of treatment as the lesions are relatively radioresistant. When a tumor is strictly confined to the intranasal cavity or ethmoid or sphenoid sinus it can be removed via an endoscopic approach. In patients with DNS, large highly vascular tumors, lesions extending into the brain, orbit or pterygopalatine fossa endoscopic removal is not feasible. The lateral rhinotomy approach is used most frequently. Radiotherapy and chemotherapy have limited success. Chemotherapy can be used in metastatic lesions. Adriamycin is the most commonly used agent. Actinomycin D, cyclophosphamide, methotrexate and vincristine are also used.


Conclusion
Sinonasal haemangiopericytomas are very rare tumors. The uncertainty of the course of the disease and rarity in the nose and paranasal sinus region interests both clinicians and pathologists. Diagnosis is based on HPE findings as the clinical presentation and the radiological findings are vague. Standard of treatment is surgical excision either by endoscopic approach or lateral rhinotomy. Radiotherapy and chemotherapy have a limited success rate. As recurrence can occur after a prolonged disease-free interval, it is essential to follow up the patient for life.
About Author –
Dr. Nagendra Mahendra, Consultant ENT Surgeon, Yashoda Hospital, Hyderabad.
DLO, DNB (ENT)
His expertise includes micro ear surgery, phono surgery / M, endoscopic surgery, endoscopic skull base surgery & cosmetic surgery, Head & Neck related surgeries including skull base surgery & laryngotracheal surgery.





 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More