Bronchoscopic Management of Primary Tracheal Tumor
Introduction:
Primary Tracheal Tumours are relatively uncommon, which often present a therapeutic challenge to the Interventional Pulmonologist. In adults approximately 90% of the primary tracheal tumours are malignant with squamous cell carcinoma being the most common diagnosis followed by adenoid cystic carcinoma 1,2. Squamous cell carcinoma predominantly occurs in men in the 6th and 7th decades with a positive smoking history 3,4. Tracheal resection remains the primary treatment of choice. Here we report a case of primary tracheal tumour in a non-smoker female, causing central airway obstruction, which was successfully treated by Interventional Pulmonologist using endobronchial surgical technique using rigid bronchoscopy.
Case Report:
A 51-year-old female presented with complaints of cough, dyspnoea on exertion and noisy breathing for the past 3 months. She is being treated as bronchial asthma with the above-mentioned complaints. She also complained to have noticed mild blood tinge in her sputum for the past one week.
History of present illness:
There was no history of weigh loss, fever or loss of appetite. Her first consultation was to the otorhinolaryngologist, who performed an indirect laryngoscope examination and noticed a nodular growth in the subglottic area. She was referred to the department of Interventional Pulmonology for therapeutic management.
Past medical history:
Her previous medical history revealed Diabetes Mellitus.
Examinations:
Her physical examination was unremarkable with a resting room air pulse oximetric saturation of 96%. Chest radiograph showed no detectable abnormality.
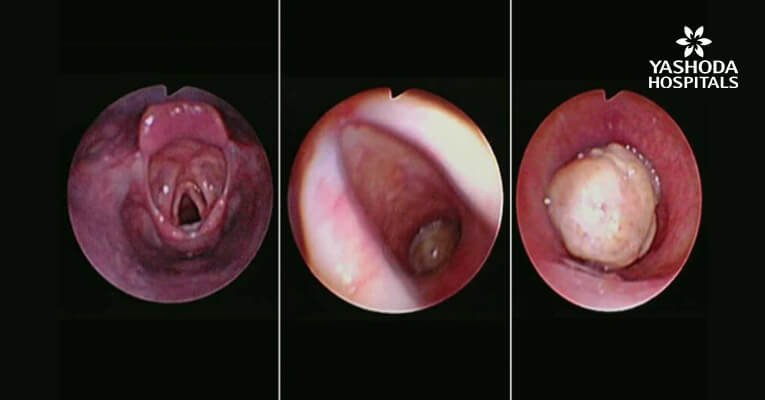
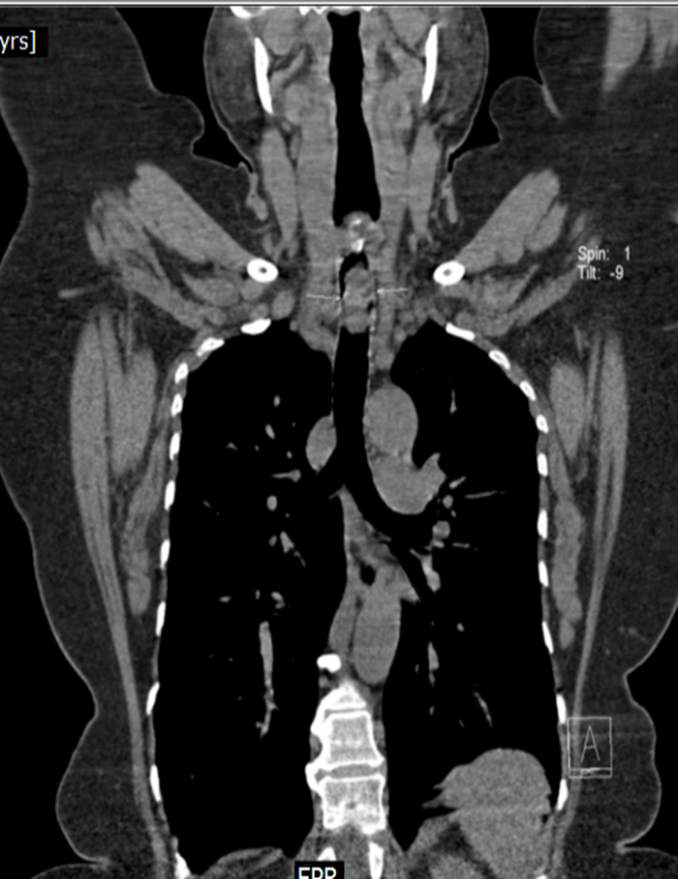
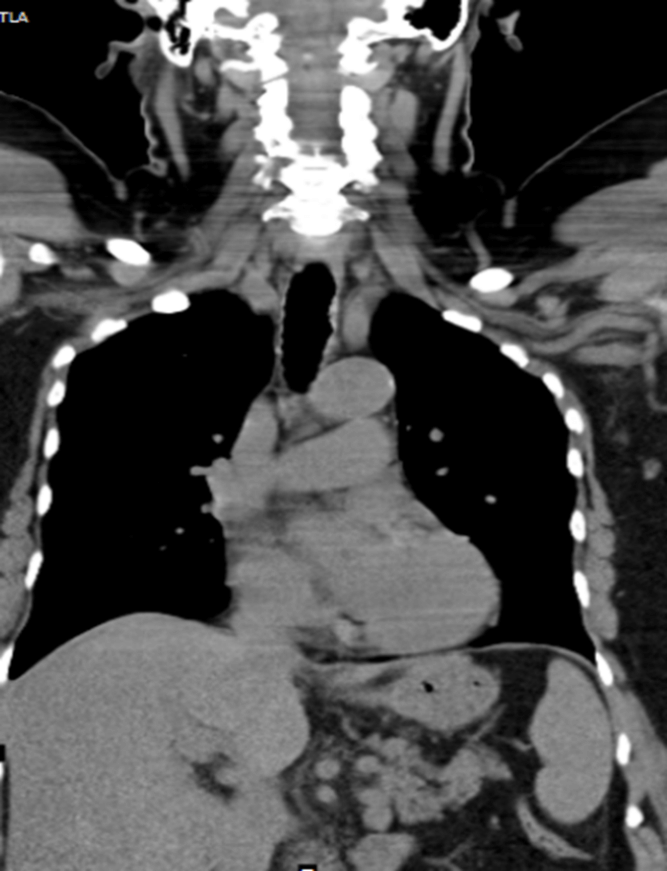
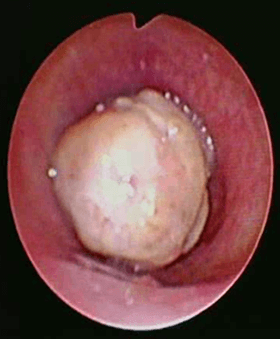
Contrast enhanced computed tomography (CECT) of neck and thorax reported intraluminal mildly enhancing polypoidal mass lesion measuring 2.58 x 1.54 x 1.51 cm (Cc X AP X Tr) in the upper trachea at the level of C6, C7 vertebral body. Significant luminal compromise was noted at the level of the mass lesion. Rest of the lung parenchyma was unremarkable. Flexible bronchoscopy examination revealed a large polyploidal growth approximately 3 cm from the vocal cords. The growth was moving with respiration and causing critical airway narrowing at the upper trachea (approximately 80%).
Diagnostic Flexible bronchoscopy Examination

Bronchoscopic Management

Bronchoscopic Management

Bronchoscopic Management
CECT at presentation: Intraluminal mass lesion in the upper trachea
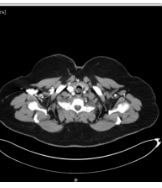
CECT at presentation

CECT at presentation

CECT at presentation
Diagnosis:
Patient had primary tracheal tumor. The tumorous growth was significantly blocking the upper trachea causing breathing difficulties and demanding immediate tumor resection.
Management:
Multidisciplinary team discussion was made with the ENT, Oncology, Anaesthesiology and Radiology departments. Decision was made to subject the patient for Rigid Bronchoscopy and mechanical debulking combined with electrosurgical snare, argon plasma coagulation and cryo-debulking using the ERBE cryoprobe under general anaesthesia.
Treatment:
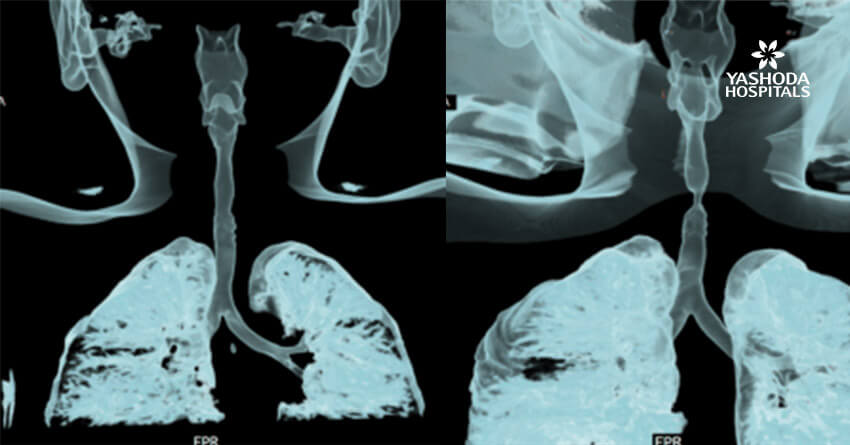
Patient was intubated using a rigid bronchoscope (EFER DUMON, 10.00/9.20 mm tracheal tube) after induction with fentanyl and propofol. The procedure was done under total intravenous anaesthesia. After successful intubation with the rigid bronchoscope, flexible bronchoscope was passed through the rigid scope. A 4mm MLS endotracheal tube with standard cuff was passed next to the rigid bronchoscope and was positioned beyond the tumour with cuff inflated at about 4 cm above the carina. This approach helps the endoscopist to have total control of the ventilation through out the procedure. Initial attempt was made to cut the stalk of the tumour using an electrosurgical snare, but was unsuccessful as the tumour was attached on to the trachea at multiple sites. Tumour destruction was performed using argon plasma coagulation probe. Non-contact APC was used initially to achieve deep coagulation and effective devitalization of the tumour. After effective coagulation, the cryoprobe was pressed in to the tumour and freezing was performed. The tumour was removed with cryo-extraction technique by repeatedly freezing the tumour and extracting it until the complete tumour is removed from the lumen of the trachea. The tumour base is coagulated using APC probe and contact tamponade with the rigid tracheoscope barrel. Patient is extubated immediately after the procedure.
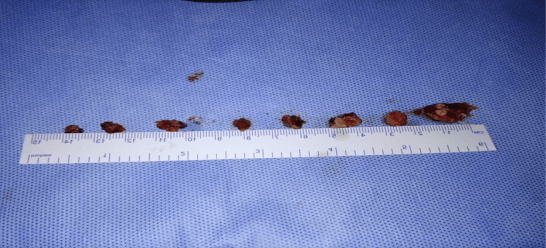
Treatment
There were no intra-operative and post-operative procedural complications. Histopathology of the tumour was reported as squamous cell carcinoma. Repeat CT post procedure revealed complete patency of the tracheal lumen with mild wall thickening and irregularity. The patient is being treated with External Beam radiation therapy by the oncology team.
Before
After
Before

After
Discussion:
Central Airway Obstruction (CAO) can result from variety of disease processes and can cause significant morbidity and mortality, especially when the cause of CAO is a malignant disease process. Primary tracheal tumours obstructing the trachea are extremely rare and pose a significant challenge in diagnosis and management. For malignant CAO, though surgery remains the standard of care in possible cases, with the advent of Interventional Pulmonology techniques, we can palliate the symptoms and perform curative endoscopic resection in selected cases. Various Interventional techniques are available includes, rigid coring, argon plasma coagulation, cryoextraction and cryotherapy, laser bronchoscopy, stent placement etc. Symptoms can range from mild shortness of breath to severe respiratory failure. Combined modality of treatment using APC, CRYO, Electrosurgery has proven to be effective in most of the cases. As with our case, we used a MLS ET tube to secure the airway, as ventilation remains a challenge during such procedures. Endoscopic management of CAO requires specialized training and should be performed only in “centres of excellence”. Bronchoscopic debulking offers a synergistic effect when combined with other cancer treatment modalities. Prior local treatment with interventional procedures can benefit patients with CAO. Interventional Pulmonology should be included in the Multimodality treatment team for malignant central airway obstruction as the first resort to provide immediate relief to the patients.
Conclusion:
Primary tracheal tumors are rare and can be a challenge to manage. Patients with obstructive tracheal tumors require immediate intervention both in terms of treating cancer and improving the quality of life. In this case study, a 51-year-old female was misdiagnosed and mistreated for bronchial asthma. The multidisciplinary team at our hospitals noticed a nodular growth which was later identified as tracheal tumor by the team of Interventional Pulmonology. The team subjected the patient to rigid bronchoscopy and mechanical debulking. The tumor was successfully removed with cryo-extraction technique by repeatedly freezing the tumor until the complete tumor was removed and the lumen of the trachea cleared. The patient has recovered completely post surgery without any eventful complications and is now undergoing exernal beam radiation therapy. The resected tumor was further investigated and confirmed to be a squamous cell carcinoma. The trache is now completely patent and the patient breaths fresh air with great relief.
References:
1. Culp OS. Primary carcinoma of the trachea. J Thorac Cardiovasc Surg1938;7:471–478
2. Ampil FL. Primary malignant tracheal neoplasms: case report and literature radiotherapy review. J
Surg Oncol 1986;33:20–23.
3. Pearson FG, Todd TRJ, Cooper JD. Experience with primary neoplasms of the trachea. J Thorac
Cardiovasc Surg 1984;88:511–516.
4. Grillo HC, Mathisen DJ. Primary tracheal tumors: treatment and results. Ann Thorac
Surg 1990;49:69– 77.
Disclaimer:
“The information contained herein is for educational purpose only and we request you to please consult a Registered Medical Practioner or Doctor before deciding the appropriate diagnosis and treatment.”
About Author –
Dr. Hari Kishan Gonuguntla, Consultant Interventional Pulmonologist, Yashoda Hospitals, Hyderabad
MD, DM (Pulmonology Medicine), Fellowship in Interventional Pulmonology (NCC, Japan)






 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More