Clinical Problem-Solving: A Complex Case of Auto-immune Myelofibrosis (AIMF)
Case Summary
A 58-year-old male from Ethiopia, presented with symptomatic anaemia 20 months ago. A bone marrow aspiration and biopsy revealed 99 percent cellularity with myeloid predominant pan-myelosis and dysplastic changes suggestive of myeloproliferative neoplasm/myelodysplastic syndrome (MPN/MDS). The patient underwent 15 cycles of Azacitidine treatment and received multiple blood transfusions. Subsequently, he was referred to India for an allogeneic stem cell transplant.
During his examination, the patient displayed a few key findings: restricted mouth opening, mild hepato-splenomegaly, proximal muscle weakness in both upper and lower limbs, and a skin rash. His blood tests showed a hemoglobin level of 4 g/dl, a white blood cell count of 3540 cells/cu mm, and a platelet count of 0.45 lakh/cu mm.
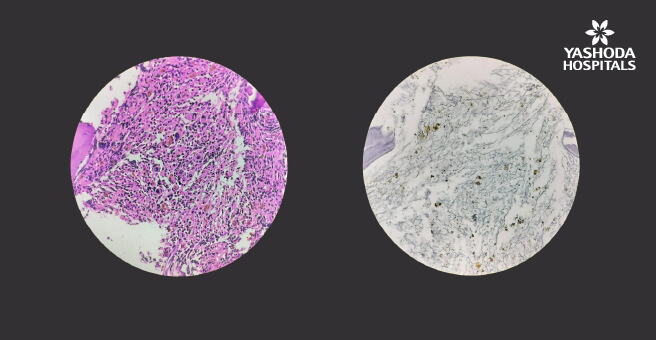
A repeat evaluation was conducted, including another bone marrow test, which demonstrated hypercellular bone marrow (90% cellularity) with normoblastic maturation in the erythroid series and normal myeloid and megakaryocytic series. While karyotyping and NGS myeloid panels yielded no abnormalities, reticulin stain showed grade 2 fibrosis. The ANA profile revealed PCNA (2+) and RNP/Sm (1+). Additionally, the myositis profile showed mi-2Beta (+), which is associated with conditions like dermatomyositis and idiopathic myositis, and PL7 (+), seen in myositis (PM, DM) with associated interstitial lung disease, systemic lupus erythematosus (SLE), and systemic sclerosis.
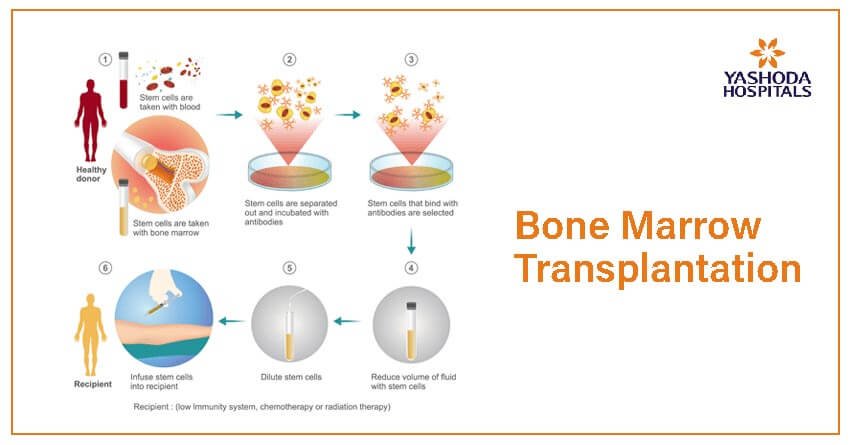
To address this condition, the patient was initiated on treatment with Corticosteroids, Rituximab, and Tacrolimus. This approach resulted in a significant improvement in symptoms, allowing him to walk without support. There was also partial improvement in his blood counts. The medical team will closely monitor his progress and make decisions about the potential need for a bone marrow transplant as needed.
Discussion
Bone marrow fibrosis (BMF) is a histologic finding in a wide range of diseases, including malignancies, endocrine disorders, autoimmune diseases, and infections. Autoimmune myelofibrosis is an uncommon etiology of BMF; it can be secondary to a defined autoimmune disease, or it can be primary in the absence of a clinically diagnosed autoimmune disease but the presence of serologic evidence of autoantibodies.
Distinguishing between primary myelofibrosis (PMF) and nonneoplastic AIMF is of the utmost importance because the prognosis and therapeutic options are different. This distinction, however, can be complicated by overlapping findings in the two disease entities. While PMF is associated with limited survival, other causes of MF, such as AIMF, appear to have a favourable clinical course.
Additional Resources
The morphologic criteria that favor AIMF rather than PMF, as proposed by Vergara-Lluri and colleagues, are the following:
- Rarity or absence of a leukoerythroblastic reaction in the peripheral blood, including absence of teardrop cells, nucleated red blood cells (RBCs), and blasts
- Absence of peripheral eosinophilia or basophilia
- Mild degree of BMF (usually MF1)
- Absence of osteosclerosis and bone changes
- Presence of hypercellular marrow characterized by erythroid and megakaryocytic hyperplasia (vs granulocytic hyperplasia in PMF)
- Presence of lymphoid aggregates, and
- Absence of dysplastic features in any of the lineages, especially the megakaryocytes
These criteria distinguish AIMF from PMF; however, the distinction can remain nebulous when not all of the criteria are met. In these scenarios, it is crucial to consider the whole clinical picture in context, including the clinical presentation, timeline of the disease course, results of assessment for autoantibodies, bone marrow pathologic findings, and results of chromosomal/genetic studies.





 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More