Acute Kidney Injury with Hemoptysis – A Formidable Challenge for a Clinician
Introduction:
Granulamatosis with polyangitis (GPA), previously known as Wegner’s granulamatosis is one of the three ANCA associated vasculitis. The pathogenesis involves an environmental trigger in a genetically susceptible individual resulting in the production of pathogenic antibodies, antineutrophil cytoplasmic antibodies (ANCAs), leading to necrotising small and medium vessel vasculitis. Early diagnosis and appropriate management are pivotal in preventing irreversible renal damage.
Case report:
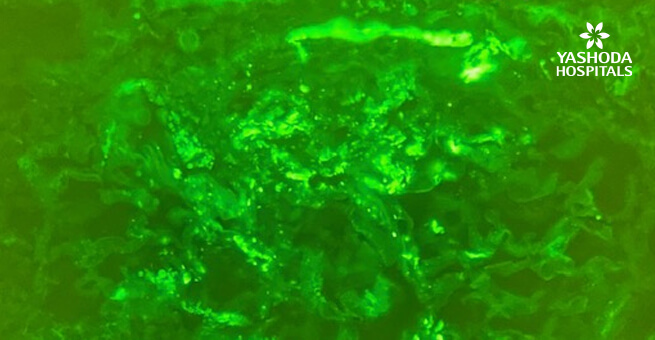
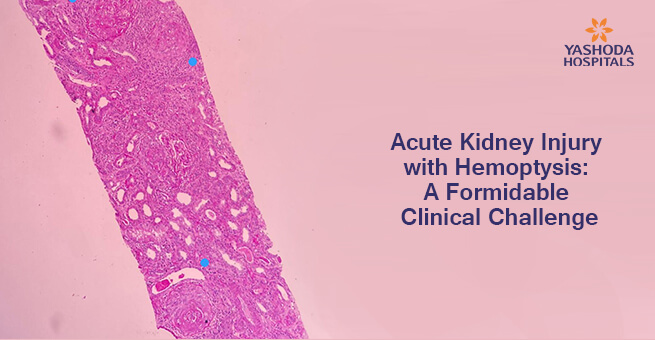
Mr. RK, 67 years, was a diabetic and hypertensive with a past present with a 4-day history of low-grade fever, cough with hemoptysis, breathlessness and decreased urine output. Evaluation on arrival showed him to be hypoxic ( SPO2- 90%), blood pressure was 150/90 mm of Hg, the temperature was 99.5 f and had pedal oedema. Laboratory examination revealed his serum creatinine to be 3.6 mg/dl, urine showed 3 + albumin with 20 to 25 RBCs/ HPF and his chest radiograph revealed nodular opacities. His coagulation workup was normal and he did not have evidence of infection. A provisional diagnosis of pulmonary-renal syndrome, most probably GPA was considered. Since he was oliguric and had severe metabolic acidosis in ABG, he was taken up for hemodialysis immediately. A renal biopsy was performed after 3 sessions of hemodialysis and it revealed necrotising granulomatosis crescentic glomerulonephritis (Fig 1 and 2) which was pauci immune on immunofluorescence studies (Fig 3). PR3- ANCA was positive. This confirmed the diagnosis of GPA. Since he had significant hemoptysis he was also administered 5 sessions of plasmapheresis. He was started on methylprednisolone and cyclophosphamide along with other supportive measures. His renal function improved over the next 3 weeks and hemodialysis was stopped. Now, 14 months after the diagnosis, he has a stable renal function with his serum creatinine being 1.9 mg/dl and is asymptomatic. He is now receiving prednisone along with Rituximab as maintenance therapy.
Discussion:
GPA presents as a pulmonary-renal syndrome in the elderly who have a history of recurrent sinusitis and/or pneumonia episodes. The pathogenic antibodies are ANCAs. In vitro studies reveal that once the neutrophils are primed by cytokines in a genetically susceptible individual, the cytoplasmic ANCAs get translocated to the cell surface. The neutrophils with ANCAs on the cell surface then bind to the antigens and get activated. These activated neutrophils infiltrate into the small and medium-sized vessel walls leading to necrotising vasculitis in the kidneys and lungs. A renal biopsy is indispensable for diagnosis, management and prognostication, and it needs to be performed as early as possible. The main stray of treatment includes immunosuppressive medications which include corticosteroids, cyclophosphamide, rituximab, azathioprine and mycophenolate. In patients with severe disease or those who present with hemoptysis, cyclophosphamide along with plasmapheresis is preferred over rituximab during remission induction. In patients who also have a concomitant anti-GBM antibody disease, plasmapheresis is essential.
Conclusion:
GPA is an aggressive disease in the elderly and needs to be diagnosed early for appropriate management. Our patient could be treated with excellent results due to the early diagnosis by renal biopsy, timely administration of methylprednisolone along with cyclophosphamide and performing plasmapheresis during the induction phase and continuing therapy with prednisone next and rituximab in the maintenance phase.
Figure 1: Core showing 3 glomeruli
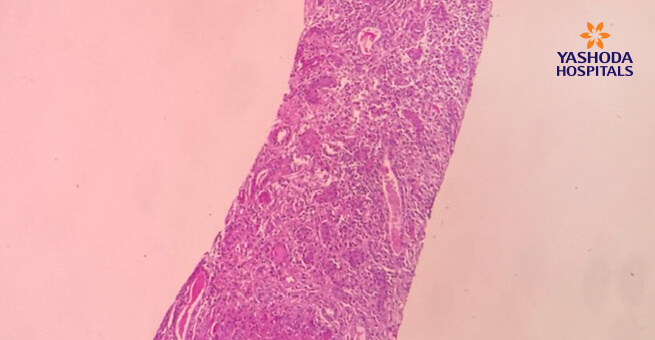
Figure 2: High power view of the glomeruli with circumferential crescent with peripheral giant cell reaction.
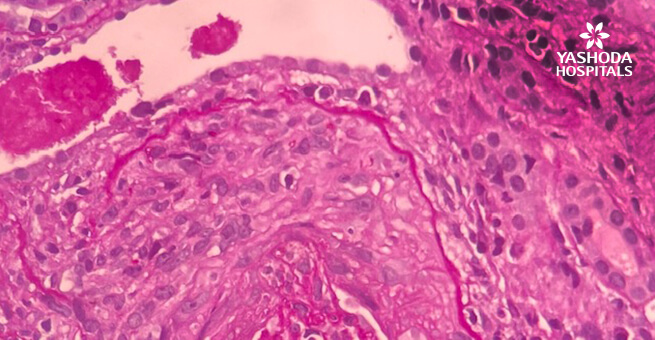
Figure 3: No immune deposits on immunofluorescence.





 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More