Varicose veins: causes, symptoms, and treatment

At a Glance:
2. What are the symptoms of varicose veins?
3. What are the causes and risk factors of varicose veins?
4. How are varicose veins diagnosed?
5. What are the treatment options for varicose veins?
6. How will a person know which procedure is right for him/her?
7. What can a person expect during varicose vein treatment recovery?
8. How should one choose a facility for the treatment of varicose veins?
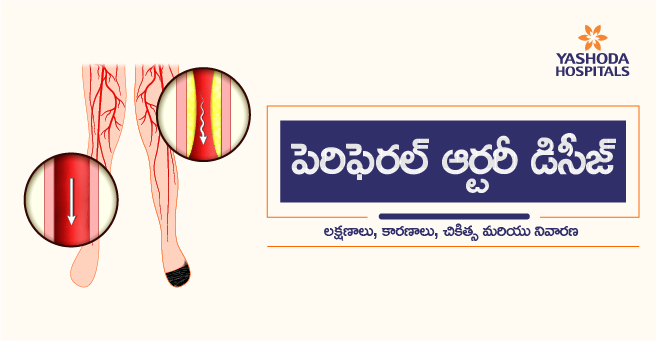
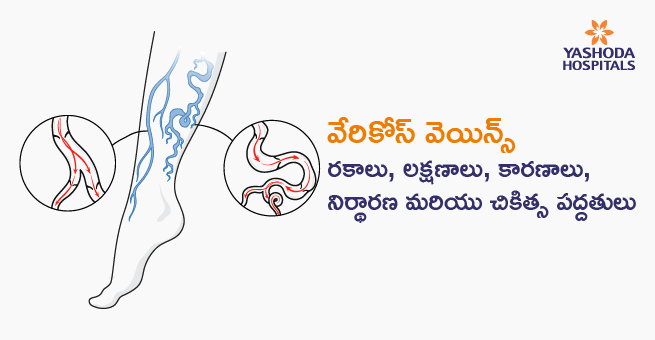
What are varicose veins?
Subcutaneous veins that become elongated, tortuous and dilate ≥3 mm in diameter are called varicose veins. Even though, superficial veins anywhere in the body can become varicosed those in the legs are most affected. The main reason the veins of the legs get affected is that walking and standing upright for a long duration increases the pressure in the veins of the lower body.
Varicose veins and one of its milder and commoner variation, the spider veins may just be a cosmetic concern for some persons. However, for some, they may be a cause of symptoms, ranging from pain to ulcers, that require prompt treatment and medical intervention.
What are the symptoms of varicose veins?
In most of the cases, varicose veins do not cause any pain. Varicose veins appear:
- Dark purple or bluish-colored
- Twisted and bulged
- Cord like in texture and feel
Symptomatic cases of varicose veins may also report with :
- A feeling of heaviness or a dull ache in the legs
- Feeling of throbbing, burning, swelling,or cramps in the lower legs
- Pain may worsen if a person stands or sits for a long time
- Persistent itchiness around one or more affected veins
- The skin around the varicose vein may get discolored
- Venous ulcers: Open, non-healing sores located low on the inner ankle, but may also occur on the outer ankle and the shin area. Venous ulcers do not occur above the knee or on the foot itself or the toes.

What are the causes and risk factors of varicose veins?
Varicose veins are caused by damage or weakening of the valves in the veins that maintain a unidirectional flow of blood from the legs to the heart against gravity. Damage or weakening of these can lead to a backward flow of blood and its pooling in the vein. As a result, the veins begin to stretch or twist.
Some common factors that increase a person’s risk of developing varicose veins are:
- Age: With advancing age,the valves may get worn away, thereby allowing the blood to flow back into the veins and start pooling.
- Gender: Women are more prone to develop the condition, probably due to hormonal changes during pregnancy or menopause that may lead to a relaxation of venous walls or due to an increased blood volume during pregnancy.
- Hereditary factors: History of varicose veins in first-degree relations increases the risk of a person developing varicose veins too.
- Obesity: Overweight individuals are at increased risk because excess weight creates added pressure on the veins.
- Standing or sitting for long duration: Remaining in the same position for long periods creates a pressure on venous valves as they have to work against gravity for a longer duration.
How to diagnose varicose veins?
A vascular surgeon can diagnose varicose veins by undertaking a person’s detailed medical history like asking about symptoms of pain and itching and conducting a physical examination. The exam includes a visual inspection of the person’s legs while standing to check for the presence of swelling or venous enlargement.
An ultrasound test is performed to see the functionality of the valves in the veins or evidence of a blood clot.
How to treat varicose veins?
The treatment for varicose veins usually does not require a hospital stay for long. Recovery is usually fast and uneventful. Due to the availability of lesser invasive procedures, varicose veins can routinely be treated on an outpatient basis, though open surgery may be required for certain persons.
Treatment goals for varicose veins are to:
- Improve symptoms and appearance
- Reduction of edema
- Improvement in skin changes
- Healing of ulcers
Some of the treatment options for varicose veins are:
Conservative management options
- Self-care: Activities such as regular physical exercising, weight loss in case of overweight persons, wearing loose-fitting clothes, periodically elevating the legs, and avoiding prolonged periods of standing or sitting can help to reduce the pain and prevent the condition from getting worse in persons with existing varicose veins.
- Compression stockings: Before physicians advise other modes of treatment, the first option is to try wearing compression stockings all day. Stockings help by steadily squeezing the legs. The veins and leg muscles can thereby move blood more efficiently.
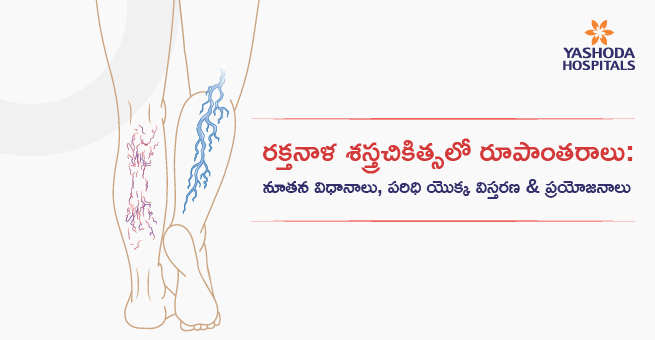
Interventional treatments for more-severe varicose veins
If a person does not experience improvement in condition with self-care or compression stockings, or if the condition of varicose veins is more severe in the vascular surgeon’s opinion, one of the interventional treatments known as vein ablation may be recommended. Several venous ablation techniques, including minimally invasive and surgical methods, are available and they are of two categories:
- Those that close the affected veins by sealing the vein so that blood cannot flow through it anymore
- Those that remove the affected veins altogether
When ablation is done, the blood that would normally flow through the affected vein gets diverted through another route back to the heart. Ablation of the veins can be done by the following techniques:
Thermal ablation: Constitutes minimally invasive methods that achieve vein-ablation by generating heat at a temperature at which the proteins within the venous wall get denatured. Radiofrequency energy or laser light is used for generating heat which is introduced into the lumen of the affected vein using specialized catheters. Heat generation within the vessel wall may result in pain. To counter it, an added infiltration of local anesthetic and saline mixture, called as tumescent anesthesia is administered. It also provides a cold buffer from the heat generated by the laser or radiofrequency energy and compresses the vein from outside to help close contact of the catheter with the vessel wall. Both the procedures are percutaneous and ultrasound-guided.

- Endovenous Laser Treatment (EVLT) or Endovenous laser ablation (EVLA): An interventional radiologist or vascular surgeon performs this procedure by using laser energy. The treatment usually takes between one to two hours and it is done in an OPD setting. Through a small puncture, a catheter bearing a laser fiber is inserted into the affected vein. The catheter is then advanced to the level of the groin and tumescent local anesthesia is administered. The vein is obliterated along its entire length as the laser is activated whilst the catheter or laser fiber is slowly withdrawn.
- Radiofrequency ablation (RFA): In this procedure, the doctor uses radiofrequency energy or radio waves to perform the ablation. A small catheter is inserted into the diseased vein through a small incision. The collagen in the vein walls contracts when consistent and uniform heat is delivered. As a result, the veins collapse and close. The treated vein is then gradually absorbed into the surrounding tissue. Laser ablation is a preferred choice in cases where the veins have a larger diameter or in cases of clots or vein webs. This is so because the contact of the catheter with the vein wall may not be adequate. However, in most cases, RFA is a preferred option because of less bruising, lower risk for perforation, and lesser postoperative pain.
Nonthermal ablation: This is an alternative technique for ablation of varicose veins with a sealing system which includes the endovenous delivery ofa wire, chemical, or glue, or a combination of these into the diseased vein instead of using heat. It can be done in an OPD setting with local anesthesia. As there is no requirement of heat, the discomfort associated with tumescent infiltration is avoided, and there is a lower risk of adjacent nerve injury. Nonthermal techniques like polidocanol endovenous microfoam [PEM], mechanochemical ablation [MOCA], cyanoacrylate glue, etc are suitable minimal invasive options for veins that are not amenable to thermal ablation. Some common types of nonthermal ablation techniques are:
- Liquid, foam, or glue sclerotherapy: In these procedures, the diseased vein is injected with a chemical or glue. As a result, the vein collapses on itself. Even though the vein stays in placeafter this procedure, it no longer carries blood. Sclerotherapy or glue therapy can be done in OPD with local anesthesia. It can be performed under direct vision or can be an ultrasound-guided procedure. Sclerotherapy is indicated for the treatment of symptomatic telangiectasias, reticular veins, and small varicose veins. The venous sclerotherapy agents are formulated either as a liquid or foam.
- Liquid preparations are used for the treatment of small nonaxial veins with cosmetic concerns.
- The foam preparations are used when the varicose and refluxing axial veins are larger than 6 mm.
- Cyanoacrylate glue: One of the latest developments in the non-thermal treatment options for varicose veins is the introduction of glue therapy with cyanoacrylate. Like radiofrequency, a catheter is placed in the vein below the knee and passed to the top of the vein near the groin. As the catheter is withdrawn, a small amount of glue is injected and held closed for a few seconds, allowing the glue to set. The affected vein is permanently closed, as it collapses and becomes like a thread of scar tissue under the skin, becoming invisible. Some of the major advantages of glue therapy are:
- Can be done under local anesthesia
- There are no pre-procedure drugs required
- A person can return to routine activities right after the treatment.
- No risk of skin burns or nerve damage, unlike thermal ablation.
- There is no need for immediate post-treatment pain medication or compression stockings.
- Mechanical occlusion chemically assisted (MOCA) ablation: This procedure is performed by using both mechanical and chemical means to do the ablation. A tube with a rotating hollow wireis used to induce damage to the inner lining or endothelium of the vein and a liquid sclerosant is simultaneously injected for chemical irritation to the vein, causing it to shrivel and close. The procedure is done using local anesthetic under ultrasound guidance. Compression stockings may be recommended to be worn for a few days after the procedure.MOCA ablation has shown the following benefits:
- With similar symptomatic relief, individuals undergoing MOCA experience less pain during and after the procedure than with radiofrequency ablation
- Successful closure is obtained in up to 95% varicose veins
- Faster recovery, a person can return to routine activities within 1–4 days
Open surgical techniques: As the minimally invasive techniques of vein ablation evolve to be the standard of care, open surgery options are reserved for the treatment of varicose vein cases that are:
- Complications of varicose veins like recurrent phlebitis and hemorrhage
- Not amenable to treatment by lesser invasive means
- Refractory or recurrent venous ulceration
- Exceptionally large varicose vein
In many cases, surgical treatment is also combined with less invasive treatment options in selected patients for better outcomes. The choice of technique whether ligation and/or removal of veins is dependent on the presence or absence of venous reflux, location, size, and extent of the affected veins.
- High ligation and vein stripping: The affected vein is tied off at a point before it joins a deep vein. The vein is then removed through small incisions. For most of the cases, the procedure is done on an outpatient basis.
- Ambulatory phlebectomy: The vascular surgeon removes smaller affected veins through a series of tiny skin punctures in this technique. Local anesthesia is administered in the parts of the leg that are being pricked. The procedure is done on an outpatient basis.
- Endoscopic vein surgery: This procedure is usually done in advanced cases of varicose veins with ulcers if other techniques do not yield desired outcomes. A thin tube with a camera is inserted through a keyhole in the leg by the vascular surgeon which helps to visualize the varicose veins. The surgeon then closes and removes the veins by inserting surgical tools through small incisions. The procedure is done on an outpatient basis.
- Transilluminated powered phlebectomy (TIPP): In this technique for vein removal a bright light is used to illuminate the vein. A device is passed through a tiny incision and the vein is removed with suction by a mechanical aspirator.
How to know which procedure is right for an individual with varicose veins?
Before selecting the appropriate procedure, certain factors need to be weighed in making that decision by the person and treating vascular surgeon. Among them, the following are important:
- Age and overall health of the person
- The extent to which the veins are affected
- Symptoms of the condition
- Ability to undergo specific procedures
- Personal needs of the individual about the appearance and feel
- Expected prognosis of the condition in the future
How to recover from varicose veins?
Once a procedure is carried out, the person may feel the procedure-specific side effects. Some of the common effects of most procedures are swelling, bruising, change in color of the skin, and pain.
The side effects of open surgical treatment like vein stripping and ligation may be more severe as compared to the less invasive options. Although they’re rare, complications of open surgery can include blood clots, severe pain, infection, and scarring at the site of the procedure.
In some techniques, the legs may need to be wrapped in elastic bandages after the procedure, and it is advised to wear compression stockings for a certain amount of time.
Postoperative instructions about physical therapy and exercise should be adhered to avoid the formation of blood clots. Recovery after a procedure for varicose vein treatment depends on the type of procedure and individual factors, but in the majority of cases, a person will be able to return to routine life within a week or two.
How to choose a facility for the treatment of varicose veins?
Treatment outcomes of varicose veins are highly technique-sensitive as each method of endovenous ablation whether thermal or nonthermal, has unique characteristics that must be taken into consideration to meet the expectations of the affected person and treating surgeon. Individualized treatment plan and comprehensive care for persons with the chronic venous disease involves a clear understanding of the technical differences and the advantages and disadvantages of each technique. Every ablation technique requires specific surgical skills that can be achieved only with experience and training. Considering that treatment for varicose veins requires a multidisciplinary approach with advanced infrastructure, treatment should be availed at a high volume center for a holistic care experience.
Conclusion:
Nonthermal or thermal vein ablation treatments for varicose veins have emerged to be an ideal option for persons who have symptoms of varicose veins that are not responsive to the conservative options. Even though long-term outcomes for open and endovenous techniques are similar, endovenous ablation is recommended as one of the primary approaches to treat symptomatic vein reflux. This is because of far lesser chances of complications, faster recovery, and cost-effectiveness of endovenous ablation techniques as compared to open surgical ligation and stripping.
The Center for Vascular Surgery at Yashoda Hospitals provides holistic care to persons with varicose veins with the following approach:
- Multidisciplinary care: The vascular surgery care team works with a multidisciplinary approach in close coordination with dermatologists trained in treating a range of skin conditions, interventional radiologists, imaging experts, and others to diagnose and treat vascular conditions.
- Advanced diagnostics: The center for vascular surgery is equipped with the necessary infrastructure and the vascular surgeons make use of detailed imaging tests to accurately diagnose varicose veins, including ultrasound and other tests.
Availability of latest treatments: Vascular surgeons at Yashoda hospital have expertise in treating varicose veins with advanced techniques that include endovenous thermal ablation including laser and radiofrequency treatment, all types of sclerotherapy, laser surgery, vein stripping, endoscopic vein surgery, and other procedures.
Reference:
- Endovenous mechanochemical ablation for varicose veins. Available at. https://www.nice.org.uk/guidance/ipg557/resources/endovenous-mechanochemical-ablation-for-varicose-veins-pdf-3228240382405. Accessed on January 26, 2020
- Mayo Clinic. Varicose veins. Available at: https://www.mayoclinic.org/diseases-conditions/varicose-veins/symptoms-causes/syc-20350643. Accessed on January 26, 2020
- Stanford Healthcare. Varicose Veins. Available at: https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/varicose-veins.html#about. Accessed on January 26, 2020














 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More