Advances in Treatment of Trigeminal Neuralgia – The Suicide Disease

What is trigeminal neuralgia?
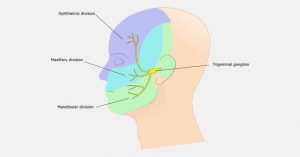
Trigeminal neuralgia, commonly known as tic douloureux, is severe facial pain rooted from disrupted functioning of trigeminal nerve. Trigeminal nerve and its branches connect the brain to the face and is responsible for touch, temperature, and pressure sensations from forehead to jaw, including inside the mouth.
Trigeminal neuralgia is experienced as severe, “stabbing or shock” like facial pain. Patients may notice aggravated pain in extreme cold or hot conditions. Trigeminal neuralgia begins as a short, mild attacks and progresses to being more frequent, lengthy and worse. Usually, the pain is one sided and can be triggered by simple everyday tasks like chewing, lightly touching the face, smiling or shaving.
Why is it called as the suicide disease?
Chronic pain can be debilitating. The pain associated with trigeminal neuralgia is arguably considered to be most disturbing form of chronic pain. Historically, it is often known as suicide disease as majority of sufferers were reported to have committed suicide. However, there is no substantial evidence to support this claim. The advances in medical field has been promising since the 1900s to treat trigeminal neuralgia.
What causes trigeminal neuralgia?
Trigeminal neuralgia is caused by enlarged blood vessel causing compression or throbbing of trigeminal nerves. This compression damages the protective myelin sheath and causes erratic and hyperfunctioning of the nerve. Trigeminal neuralgia may also be attributed to:
- Multiple sclerosis
- Brain lesions or abnormalities in the CP angle
- Stroke
- Trauma – surgical injuries, facial trauma, accidents
- Lupus
- Herpes zoster
- Scleroderma
Who is more likely to get trigeminal neuralgia?
Risk factors for trigeminal neuralgia include:
- Family history
- Ageing: more commonly see in people of age above 50 years.
- Gender: Trigeminal neuralgia is seen in women more than men.
- High blood pressure
What are the symptoms of trigeminal neuralgia?
The symptoms of trigeminal neuralgia include:
- Severe “stabbing, shooting, shock like”pain attacks
- Pain in the cheek, teeth, gums, jaw, lips, eyes or forehead
- Pain may last for a few minutes
- Pain may occur several times a day or week and may be silent for a while
- In some patients, anxiety of pain during pain free periods
- Patients do not experience pain during sleep
Classic trigeminal neuralgia is marked by sudden and severe episodes of pain. However, if the pain is less intense but is like consistent aching or burning sensation, then it is due to atypical terminal neuralgia.
When to see a doctor?
See the doctor when the facial pain does not subside with over-the-counter pain killers or when the pain is recurring or worsening in intensity or duration.
Remember to tell the doctor about – triggers of facial pain, its severity and how often do the pain attacks occur and last.
How is trigeminal neuralgia diagnosed?
Facial pain may occur due to many reasons. Often, trigeminal neuralgia is misdiagnosed for migraine, post-herpetic neuralgia, cluster headache, temporomandibular joint disorder.
To confirm trigeminal neuralgia, a neurologist classes the pain based on type, location and triggers of facial pain. Reflex tests and neurological examination with an MRI is mandatory to determine whether it is neurovascular conflict, multiple sclerosis or a tumor that is causing trigeminal neuralgia.
What are the treatment options available?
Patients diagnosed with trigeminal neuralgia are treated with medications as a first line of care. They include anticonvulsants to block painful stimuli from going into the brain and muscle relaxants to reduce the influence of neurovascular conflict. Also, doctor may prescribe medicines for depression and anxiety.
In general, trigeminal neuralgia is progressive and may become non-responsive to medication. Sometimes, the medicines may themselves cause side effects that lead to cessation of medicine use. In such cases, doctors recommend surgical or minimally invasive interventions; radiofrequency ablation, microvascular decompression, and stereotacic radiosurgery.
Radiofrequency ablation:
Radiofrequency (Rf) ablation is a minimally invasive, safe and effective procedure which is used as primary treatment for drug resistant trigeminal neuralgia. The outcomes are comparable to that of microvascular decompression. Rf ablation has become the procedure of choice nowadays, more so for the patients who are old and are at high risk for anesthesia. This procedure selectively destroys nerve fibers associated with pain using radiofrequency electrical signal.
Under sedation, neurosurgeon inserts and guides a hollow needle to the trigeminal nerve. Then, the patient is awakened from sedation. An electrode is passed through the needle and a mild signal is applied to confirm the pain location. Once the target nerve fiber is confirmed, the patient is sedated again for radiofrequency thermal lesioning. The neurosurgeon selectively heats the nerve fiber by heating the electrode until the nerve fiber is destroyed and a lesion area is formed. The patient may feel facial numbness for a few hours after the procedure.
Microvascular decompression:
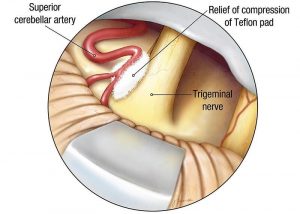 Microvascular decompression involves isolation of blood vessels that are compressing the trigeminal nerve. The blood vessel is either relocated or removed from the contact with the affected trigeminal nerve.
Microvascular decompression involves isolation of blood vessels that are compressing the trigeminal nerve. The blood vessel is either relocated or removed from the contact with the affected trigeminal nerve.
The neurosurgeon makes a cut behind the ear on the side of pain. Then, a small hole in made in the skull. The surgeon moves the arteries along the trigeminal nerve away and cushions the space between nerve and arteries.
Microvascular decompression has good success rate most of the time, however, the pain may recur in some cases. Patients do not experience any facial numbness as seen in radiofrequency ablation. However, there are chances of decreased hearing, facial weakness, stroke or other complications.
Stereotactic radiosurgery:
Stereotactic radiosurgery is a non-invasive radiotherapy with good success rates. In this procedure, the neurosurgeon makes use of highly focused beam of radiation to damage the target trigeminal nerve fiber. The pain relief is noticed gradually after a few weeks post radiosurgery. In case the pain recurs, the procedure may be repeated.
References:
- Mayo clinic. Trigeminal neuralgia. Available at: https://www.mayoclinic.org/diseases-conditions/trigeminal-neuralgia/symptoms-causes/syc-20353344. Accessed on April 19, 2018.
- Trigeminal Neuralgia (Tic Douloureux). Available at: https://www.health.harvard.edu/pain/trigeminal-neuralgia-tic-douloureux- Accessed on April 19, 2018.
- WebMD. What Is Trigeminal Neuralgia? Available at: https://www.webmd.com/pain-management/guide/trigeminal-neuralgia#1 Accessed on April 19, 2018.
About Author –
Dr. Ravi Suman Reddy, Senior Neuro & Spine surgeon, Yashoda Hospitals – Somajiguda
Mch (NIMHANS), Advanced training in Stereotactic Radio-surgery (Brain Lab Academy – Germany). His expertise include frameless stereotactic neurosurgery, minimal invasive spine surgery, spine stabilization, cranial micro neurosurgery, cranio-spinal trauma, endoscopic surgery.
[yashoda id=”13186″ _builder_version=”3.0.47″][/yashoda]












 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More