Portal hypertension and TIPS (Transjugular Intrahepatic Portosystemic Shunt)
At a Glance:
1. What is portal hypertension?
4. What can one expect before a transjugular intrahepatic portosystemic shunt procedure?
5. How is the TIPS procedure done?
6. What happens after the TIPS procedure?
7. What are the benefits of transjugular intrahepatic portosystemic shunt?
8. What are the risks and complications of transjugular intrahepatic portosystemic shunt procedure?
9. What are the limitations of transjugular intrahepatic portosystemic shunt?
10. How should one choose a facility for transjugular intrahepatic portosystemic shunt procedure?
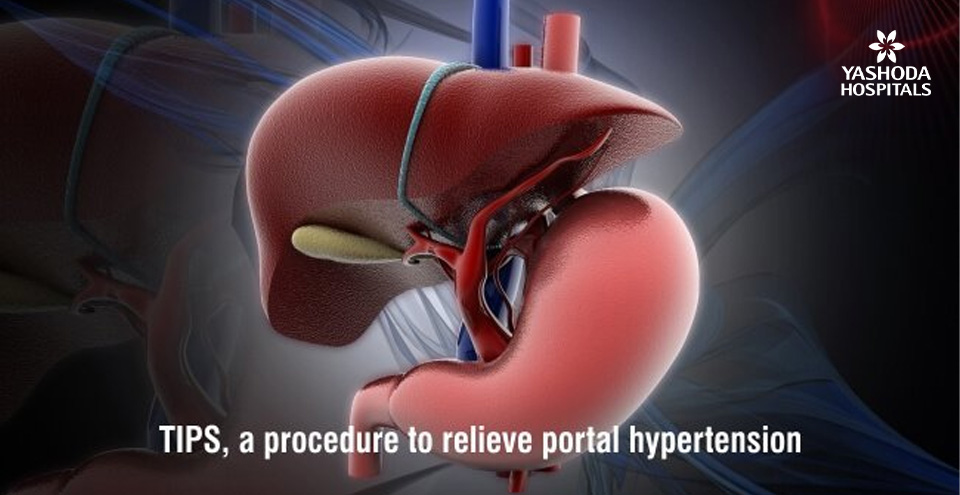
What is portal hypertension?
Portal hypertension is an increase in the pressure within the portal vein (the vein that carries blood from the digestive organs to the liver). This pressure build-up can cause blood to flow backward from the liver into the veins of the spleen, stomach, lower esophagus, and intestines, causing the blood vessels to become enlarged and susceptible to bleeding. The backward build-up of pressure also causes an accumulation of fluid in the chest or abdomen. Adults commonly get affected with portal hypertension due to chronic problems that lead to cirrhosis of the liver.
What is transjugular intrahepatic portosystemic shunt (TIPS) and how does it help in portal hypertension?
A shunt is an artificial connection that allows fluid to move from one part of the body to another. Transjugular intrahepatic portosystemic shunt (TIPS) is an artificially created connection between two veins in the liver. It connects the portal or hepatic portal vein that brings blood from a person’s gastrointestinal tract and the intra-abdominal organs namely gallbladder, pancreas and spleen to the hepatic vein that drains blood from the liver into the right part of the heart.
The transjugular intrahepatic portosystemic shunt (TIPS) procedure is performed using x-ray guidance by an interventional radiologist and the shunt is kept open by the placement of a tubular metal device known as a stent.

What are some common indications of transjugular intrahepatic portosystemic shunt (TIPS) procedure?
Portal hypertension: Typically, TIPS is performed in persons with increased pressure in the portal vein system, a condition known as portal hypertension. TIPS is particularly beneficial in the following complications of portal hypertension:
- Variceal bleeding: Veins that normally drain the gastrointestinal organs such as the stomach, esophagus, or intestines into the liver are susceptible to variceal bleeding. TIPS is done when acute variceal bleeding does not get controlled by standard treatment, to prevent recurrent episodes of variceal bleeding or to treat variceal bleeding while someone is awaiting a liver transplant.
- Portal gastropathy: Severe bleeding can also be caused due to engorgement of the veins in the wall of the stomach.
- Severe ascites or hydrothorax: Accumulation of a pale yellow and clear liquid known as serous fluid in the abdomen and/or in the chest.
Budd–Chiari syndrome: Caused by a blockage of the hepatic veins that drain the liver, Budd-Chiari syndrome is an exceedingly rare condition. The presence of the syndrome is suspected if there is a classical triad of abdominal pain, ascites, and liver enlargement.
What can one expect before a transjugular intrahepatic portosystemic shunt procedure?
To ensure optimized treatment outcomes, an accurate diagnosis of the condition and assessment of the person for whom the procedure is indicated is essential. A preoperative evaluation is done by the treating doctor based on the following investigations and information:
Clinical history and physical examination: During the first consultation with the interventional radiologist (IR), he or she will review the person’s medical history and recommend relevant investigations.
A brief physical examination will be performed at the time of the consultation. If the IR determines that the person is a suitable candidate for the procedure, he or she will be explained the instructions to be followed before the procedure.
Before the procedure: The doctor would recommend specific preparatory instructions depending on the person’s medical status. Some of the preparatory instructions recommended are as follows:
- Pre-anesthetic checkup to determine fitness for anesthesia
- A liquid diet for a day or two days before the procedure.
- To clear the gastrointestinal tract of food products, it is recommended not to eat or drink anything for at least 12 hours before the procedure.
- The doctor’s instructions about any prescription medication that a person may be on should be adhered to. For example, if a person is on an anticoagulant or antiplatelet medication, he/she may be recommended to stop it before the procedure.
- The person may be placed on antibiotics before the procedure.
- Any allergies should be disclosed to the treating doctor during the medical history.
- Women should always inform the IR if they are pregnant. Some of the imaging tests are not recommended to be performed during pregnancy as the fetus may get exposed to the radiation too. The IR may need to take special precautions to minimize radiation exposure to the baby.
- The person can expect to stay overnight at the hospital for one or more days.
- A person is asked to sign a consent for the procedure.
How is the TIPS procedure done?
TIPS is an image-guided, minimally invasive procedure that is performed by a radiologist who is specially trained in interventional radiology, a sub-specialty within radiology. The procedure is done in a radiology suite or occasionally in the operating room. Sometimes, the procedure may be required to be done under general anesthesia, while in some cases it can be performed under sedation and monitored anesthesia care. The procedure is performed as follows:
- The person is positioned on the back.
- Monitors that track vital parameters like heart rate, blood pressure, oxygen level, and pulse are attached to the body.
- An intravenous (IV) line into a vein in the hand or arm to administer a sedative is inserted by the nursing staff if the procedure is being done by sedation. An intravenous (IV) sedative is administered so that the person feels relaxed and comfortable during the procedure. When the needle is inserted into the vein for the IV line and when the local anesthetic is injected, a slight pinch may be felt.
- The surface of the body where the catheter is to be inserted is sterilized and covered with a surgical drape.
- An area just above the right collarbone is numbed with a local anesthetic. Once numb, a very small incision or cut is made at the site.
- The IR will then locate the internal jugular vein using ultrasound. The vein is situated above the collarbone. A catheter, which is essentially a long, thin, hollow plastic tube is then inserted into the vessel.
- Once inserted in the vein, the IR then advances the catheter towards the liver into one of the hepatic veins under real-time x-ray guidance.
- The diagnosis of portal hypertension is confirmed by measuring the pressures in the hepatic vein and right heart. This also helps to assess the severity of the condition.
- A contrast dye material is injected in the hepatic vein to trace the portal venous system and plan for the placement of the TIPS stent. A person may feel some warmth as the contrast material passes through the vein.
- The portal system is then accessed from the hepatic vein using a TIPS needle that is a special long needle which is long enough to extend from the neck into the liver. The external directional indicator on the needle helps to puncture the portal vein and the needle creates a pathway for the stent. The person may feel a slight discomfort as the needle is advanced through the liver and the pathway is expanded by the balloon. The IR should be informed if the pain becomes intolerable as so extra intravenous medications may be given.
- The IR then places a stent that extends from the portal vein into the hepatic vein under fluoroscopy. The stent is placed over a balloon-tipped catheter which is advanced through the TIPS needle. Once the stent reaches the intended position, the balloon is inflated and the stent gets expanded into place.
- The balloon is then deflated and it is removed along with the catheter.
- The pressure within the vein is measured to confirm a reduction in portal hypertension.
- Additional portal venograms are done to ensure that there is satisfactory blood flow through the shunt.
- Once the procedure is completed, the pressure is applied at the site of the incision to prevent excess bleeding. The site is bandaged and no sutures may be required.
- It usually takes an hour or two to perform the procedure, but in certain cases, it may take up to several hours if the condition or the vascular anatomy is complex.
What happens after the TIPS procedure?
Once the procedure is done, the medical team monitors the person closely. The head is to be kept elevated for a few hours once a person returns from the procedure room. In most cases, since the procedure is done electively and severe complications are not experienced, a person may be allowed to go home the next day. Individuals experiencing excess bleeding are monitored in intensive care during recovery and maybe kept under observation for a longer duration in the hospital.
In the case of a non-complicated procedure, one can resume normal activities in one to two weeks.
A person may be required to undergo ultrasounds before discharge from the hospital and during follow-up after the TIPS procedure to ensure that it remains open and functions properly.
What are the benefits of transjugular intrahepatic portosystemic shunt?
TIPS is designed and expected to produce physiological results similar to a surgical bypass or shunt without the risks associated with open surgery. Consequently, it offers the following benefits
- Being a minimally invasive procedure, TIPS has a shorter postprocedural recovery time than open surgery.
- As the procedure is not transabdominal, i.e the abdomen is not entered, there is no surgical scar tissue formed in the abdomen, unlike the open surgical bypass. Consequently, the prospects of future liver transplantation surgery due to abdominal scarring are not compromised.
- The TIPS stent is placed entirely within the diseased liver. When a transplant procedure is performed, it gets removed with the liver itself and does not require a separate procedure for stent removal.
- As per available scientific literature, the TIPS procedure is successful in reducing variceal bleeding in >90 percent of persons.
- The procedure can be performed with the smallest possible incision and does not require any stitches.
What are the risks and complications of transjugular intrahepatic portosystemic shunt procedure?
Any medical procedure that requires the placement of an instrument like a needle or catheter inside a blood vessel is not devoid of any risks. Such risks include:
- Damage to adjacent structures: The possibility of complications like physical damage to the blood vessel or adjacent tissues that may cause bruising or bleeding at the puncture site, and/or subsequent infection. Usually, the doctor will take precautions to mitigate these risks, however, if still a complication happens it can cause:
- Fever
- Stiffness of the neck muscles
- Allergic reaction: Sometimes a person may experience an allergy to the contrast material used. Individuals with poor kidney health may get temporary or permanent kidney failure due to the contrast material used.
Even though they are far too less, serious complications may include:
- Cardiac complications like arrhythmias and heart failure
- Damage to the hepatic artery, that may lead to severe liver injury or bleeding requiring emergency management
- Hepatic encephalopathy or confusion
- Infection of the stent
- Injury to the skin due to radiation exposure if the procedure is complex and lengthy requiring extended fluoroscopy
- Stent blockage leading to recurrence of symptoms
What are the limitations and contraindications of transjugular intrahepatic portosystemic shunt procedure?
For persons with advanced liver disease the risk of worsening of liver failure after TIPS is high, hence a TIPS may not be the best option for persons with serious liver disease and an alternative may be needed to control the symptoms. Such persons are also prone to encephalopathy i.e. alteration of the normal brain function that can lead to confusion. Encephalopathy occurs due to the accumulation of toxic substances in the bloodstream and brain that are ordinarily filtered out by the liver. TIPS may worsen encephalopathy by bypassing these toxins from the liver.
Conditions in which TIPS is contraindicated include:
- Heart failure
- Multiple hepatic cysts
- Severe pulmonary hypertension
- Severe tricuspid regurgitation
- Uncontrolled systemic infection or sepsis
- Unrelieved biliary obstruction
Conditions in which TIPS is relatively contraindicated include:
- Hepatoma
- Moderate pulmonary hypertension
- Obstruction of all hepatic veins
- Portal vein thrombosis
- Severe coagulopathy
- Thrombocytopenia (<20,000/mm3)
How should one choose a facility for transjugular intrahepatic portosystemic shunt procedure?
Considering the need for sophisticated equipment, infrastructure, and considerable interventional radiology expertise, a transjugular intrahepatic portosystemic shunt procedure is recommended to be performed in specialized centers. Long term follow up to evaluate the performance of the procedure is a well-coordinated activity in such centers. The transjugular intrahepatic portosystemic shunt procedure technique requires experience and attention for performing the procedure under radiological guidance. This is one of the primary reasons that it is not performed in all centers. Very few interventional radiologists are trained to perform the procedure.
Yashoda Institute of Interventional Radiology in Hyderabad is a high-volume tertiary referral center for interventional radiology procedures like transjugular intrahepatic portosystemic shunt procedure. Our expert IRs often treat patients who are turned away by less experienced centers as being too risky or complex.
Conclusion:
Transjugular intrahepatic portosystemic shunt (TIPS) is a minimally invasive endovenous procedure that involves the creation of a low-resistance channel between the hepatic vein and the part of the portal vein within the liver. The procedure is performed by an interventional radiologist using radiological and angiographic techniques. The patency of the channel is maintained by placing an expandable metal stent across it, thereby allowing the blood to return to the systemic circulation by bypassing the liver. The ability of TIPS to function as a surgical bypass without open surgery, reroute blood flow in the liver and reduce abnormally high blood pressure in the veins of the stomach, esophagus, bowel, and liver has led to its rapid acceptance into clinical practice.
Reference:
- Clinical practice guidelines. Quality Improvement Guidelines for Transjugular Intrahepatic Portosystemic Shunts. Available at. https://www.jvir.org/article/S1051-0443(15)00960-4/pdf.Accessed on January 31, 2020
- org. Transjugular Intrahepatic Portosystemic Shunt (TIPS). Available at: https://www.radiologyinfo.org/en/info.cfm?pg=tips. Accessed on January 31, 2020
- S. National Library of Medicine. Transjugular intrahepatic portosystemic shunt (TIPS) Available athttps://medlineplus.gov/ency/article/007210.htm. Accessed on January 31, 2020
About Author –
Dr. Suresh Giragani, Consultant Neuro & Interventional Radiologist, Yashoda Hospitals – Hyderabad
MD (Radiology), DM (Neuroradiology)
Specialized in the comprehensive and widest range of vascular interventions covering neuro interventions, hepatobiliary interventions, venous, peripheral vascular interventions and interventions in cancer care.










 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More