The Comprehensive Pneumonia Handbook: Your Ultimate Guide
Pneumonia is a common but potentially serious respiratory infection that affects millions of people worldwide. It can range from a mild illness to a life-threatening condition, making it crucial to understand its symptoms, causes, and treatment options. Hence, World Pneumonia Day annually serves as a reminder, bringing attention to the considerable global impact of this respiratory infection.
What is Pneumonia?
Pneumonia is an inflammatory condition that affects the tiny air sacs in the lungs called alveoli. These air sacs can become filled with fluid or pus, leading to symptoms like cough, fever, and difficulty breathing. Pneumonia can be caused by various microorganisms, including bacteria, viruses, and fungi.
Causes and Risk Factors
- Infection: Infections by bacteria, viruses, or fungi are primary causes of pneumonia.
- Weakened Immune System: People with weakened immune systems, like the elderly, infants, or those with chronic illnesses, are more susceptible.
- Smoking: Smoking damages the lungs’ natural defenses and can increase the risk of pneumonia.
- Chronic Diseases: Conditions like COPD, diabetes, and heart disease can make individuals more vulnerable to pneumonia.
- Environmental Factors: Exposure to pollutants, such as asbestos or excessive air pollution, can also increase the risk.
Symptoms:
- High fever
- Cough, which may produce mucus
- Shortness of breath
- Chest pain
- Fatigue
- Confusion (especially in older adults)

Diagnosis : If pneumonia is suspected, a healthcare provider will typically perform a physical examination, chest X-ray, and may request blood tests or sputum tests to confirm the diagnosis and identify the causative agent.
Treatment : The treatment approach for different types of pneumonia varies. Bacterial pneumonia typically requires antibiotics as the primary treatment. In the case of viral pneumonia, antiviral medications may be utilized for specific viral infections, although rest, fluids, and supportive care are often the main recommendations. Fungal pneumonia is treated with antifungal medications. Aspiration pneumonia, on the other hand, involves addressing the underlying cause, which may include antibiotic therapy.

Prevention
- Vaccination: Vaccines are available for some of the common bacteria and viruses that cause pneumonia, including the flu vaccine and the pneumococcal vaccine.
- Good Hygiene: Practicing proper handwashing and respiratory hygiene can help reduce the spread of germs.
- Smoking Cessation: If you smoke, quitting can reduce your risk of pneumonia and other lung diseases.
- Healthy Lifestyle: Maintaining a strong immune system through a balanced diet, regular exercise, and adequate sleep can also help.
Types and Classifications
Classification Based on Causative Agents
Pneumonia can be classified into several categories based on the causative agents responsible for the infection. The most common classifications are:
- Bacterial Pneumonia: This type of pneumonia is primarily caused by bacteria, with streptococcus pneumoniae being the most common culprit. Other bacteria such as Haemophilus influenzae and Staphylococcus aureus can also lead to bacterial pneumonia.
- Viral Pneumonia: Viruses, including the influenza virus, respiratory syncytial virus (RSV), and the coronavirus responsible for COVID-19, can cause viral pneumonia. This type of pneumonia often presents with flu-like symptoms and can be particularly severe.
- Fungal Pneumonia: Fungal pneumonia is less common and typically affects individuals with weakened immune systems. Fungi like Candida, Aspergillus, and Histoplasma can lead to fungal pneumonia.
Aspiration Pneumonia: This type of pneumonia occurs when foreign substances, such as food, stomach acid, or saliva, enter the lungs. Aspiration pneumonia is more common in people with swallowing problems or those who have experienced a near-drowning event.

Classification Based on Location
- Lobar Pneumonia: Lobar pneumonia affects one or more lobes of a lung. It often presents with distinct consolidation of lung tissue in a specific area, resulting in symptoms like high fever, chest pain, and productive cough.
- Bronchopneumonia: Bronchopneumonia is characterized by the inflammation and infection of small airways and bronchioles, rather than whole lobes. It often appears as patchy infiltrates on a chest X-ray and may result from various causative agents.
Community-Acquired vs. Hospital-Acquired Pneumonia
- Community-Acquired Pneumonia (CAP): CAP is contracted in non-healthcare settings, such as the community, at home, or in public places. Streptococcus pneumoniae is a common cause of CAP, but the specific causative agent may vary depending on factors like age and underlying health conditions.
- Hospital-Acquired Pneumonia (HAP): HAP is acquired during a hospital stay or within a healthcare facility. Patients in intensive care units (ICUs) or those on mechanical ventilation are at higher risk. HAP is often caused by drug-resistant bacteria.
Atypical vs. Typical Pneumonia
- Typical Pneumonia: Typical pneumonia is characterized by the classic symptoms of high fever, productive cough, and pleuritic chest pain. It is often caused by bacteria and responds well to antibiotic treatment.
- Atypical Pneumonia: Atypical pneumonia, caused by atypical pathogens like Mycoplasma pneumoniae and Chlamydophila pneumoniae, often presents with milder symptoms such as a dry cough and low-grade fever. It may require different antibiotics or antiviral medications.
Other types of Pneumonia
- Necrotizing Pneumonia: Necrotizing pneumonia is a severe form with lung tissue destruction. It is often caused by aggressive bacteria like Staphylococcus aureus, requiring prompt antibiotic treatment and sometimes surgical intervention.
- Persistent Pneumonia: Persistent pneumonia doesn’t resolve as expected and may need further investigation through tests like bronchoscopy or lung biopsy to identify underlying issues, with treatment tailored accordingly.
- Usual Interstitial Pneumonia Treatment: Usual interstitial pneumonia (UIP) is treated with medications like corticosteroids or immunosuppressive drugs to manage inflammation and, in severe cases, lung transplantation may be considered.
Identifying Specific Bacteria and Organisms
- Streptococcus pneumoniae: Streptococcus pneumoniae, also known as pneumococcus, is the primary cause of pneumonia. The quellung reaction, a biochemical test, uses specific antibodies to detect its unique capsule, aiding in treatment selection due to antibiotic resistance concerns.
- Klebsiella pneumoniae: Klebsiella pneumoniae, a common cause of pneumonia in healthcare facilities, is prone to antibiotic resistance. The Indole Test is vital for distinguishing it from other bacteria, helping clinicians choose the right antibiotics.
- Mycoplasma pneumoniae: Mycoplasma pneumoniae causes “walking pneumonia” and lacks a cell wall, making traditional antibiotics ineffective. Diagnosis involves molecular and serology tests rather than traditional biochemical methods.
- Adenovirus Pneumonia: Adenovirus can cause pneumonia, especially in children. Diagnosis relies on clinical symptoms and laboratory tests like PCR for viral DNA and antigen tests for viral proteins in respiratory samples.
- Pneumocystis Jirovecii: Pneumocystis jirovecii affects immunocompromised individuals. Diagnosis involves molecular tests and microscopic examination of respiratory samples as it doesn’t respond to antibiotics.
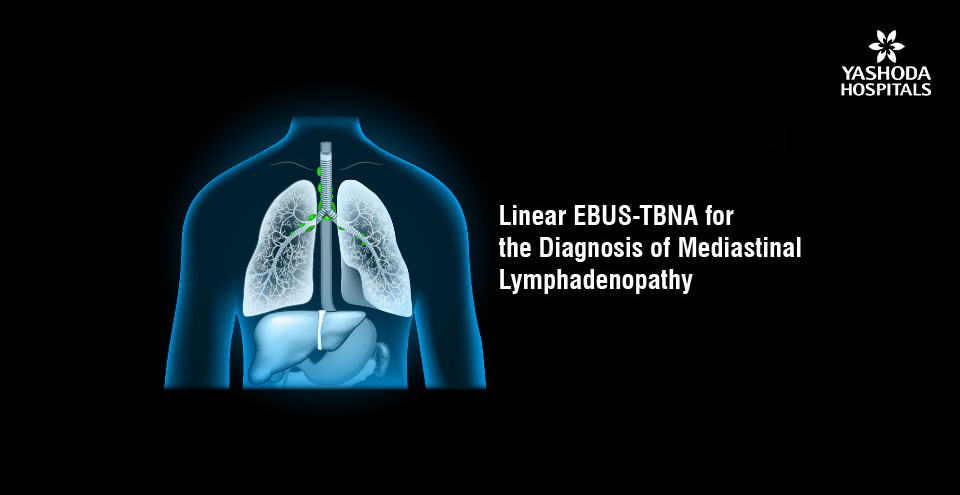
The Role of X-Rays in Diagnosing Pneumonia
While biochemical tests are indispensable for identifying specific pathogens, X-rays play a pivotal role in diagnosing pneumonia, regardless of the causative agent. They provide a visual assessment of lung health and can reveal characteristic patterns associated with pneumonia. For instance, X-rays may show infiltrates, consolidation, or the “butterfly” appearance indicative of Klebsiella pneumoniae infections. This radiological evidence aids in confirming the diagnosis and assessing the severity of the condition.
Facing pneumonia uncertainties? Get personalized guidance. Your health matters – seek a consultation now.
Post-COVID Pneumonia and Complications
Overview : Pneumonia typically arises in patients who have previously contracted the SARS-CoV-2 virus and have seemingly recovered from the initial infection. This secondary pneumonia can manifest in various forms, including viral, bacterial, or fungal infections. It often presents with symptoms such as persistent cough, shortness of breath, fever, and chest pain.
Complications Associated with Post-COVID Pneumonia:
- Lung Scarring (Fibrosis): Pneumonia can cause lung tissue damage and scarring, resulting in reduced lung function and long-term breathing difficulties.
- Blood Clots: Pneumonia can increase the risk of blood clot formation, which can lead to serious conditions like pulmonary embolism.
- Secondary Infections: Weakened immune systems in post-COVID patients can make them susceptible to secondary infections, such as bacterial superinfections, often necessitating intravenous antibiotics for pneumonia treatment.
- Ventilator-Associated Pneumonia (VAP): Patients who require mechanical ventilation are at an increased risk of developing VAP, a form of pneumonia that often requires intravenous antibiotic therapy for effective treatment.
- Respiratory Complications: Prolonged lung inflammation can result in ongoing respiratory symptoms, including chronic cough, exercise intolerance, and decreased lung capacity, sometimes requiring intravenous antibiotics for severe cases.
Diagnosis and Management : Accurate diagnosis of post-COVID pneumonia and its complications typically involves imaging studies, such as chest X-rays or CT scans, and clinical evaluation. Management may include supportive care, oxygen therapy, and appropriate intravenous antibiotic or antifungal treatment to address bacterial or fungal infections, as well as rehabilitation to improve lung function.
Prevention : To reduce the risk of post-COVID pneumonia and associated complications, it’s important to follow recommended COVID-19 prevention measures, including vaccination, mask-wearing, and good hand hygiene. For individuals who have already contracted COVID-19, proper monitoring and follow-up care, including intravenous antibiotic administration for pneumonia if necessary, are essential.
Diet and Nutrition During Pneumonia
When dealing with pneumonia, it’s essential to focus on a nutritious and balanced diet to support your body’s recovery. Here’s what to consider in your pneumonia diet:

Foods to Eat:
- High-Protein Foods: Lean meats, poultry, fish, eggs, and plant-based protein sources like beans, tofu, and nuts. Protein is essential for tissue repair and immune function.
- Whole Grains: Opt for whole grains like brown rice, quinoa, whole wheat bread, and oats. These provide sustained energy and essential nutrients.
- Dairy or Dairy Alternatives: Milk, yogurt, and fortified dairy alternatives can help meet your calcium and vitamin D needs for bone health.
- Clear Broths: Chicken or vegetable broths can be soothing and provide hydration and essential nutrients. They are especially good if you have a reduced appetite.
- Herbal Teas: Warm herbal teas, such as ginger or chamomile, can help soothe your throat and provide fluids.
- Honey: Honey has natural antimicrobial properties and can be soothing. You can add it to tea or consume it directly (note: honey is not suitable for infants under one year old).
Ever wondered what the best fruits for pneumonia patients are? They should consume fruits that are rich in vitamins and antioxidants that can aid recovery and boost the immune system. Citrus fruits like oranges and lemons are rich sources of Vitamin C, which helps to fight against infections. Berries such as strawberries and blueberries are packed with antioxidants and vitamins that support overall health. Pineapple is likewise useful due to its anti-inflammatory properties and high vitamin content. Including these fruits in the diet can help to enhance immune function and promote faster recovery.

Foods to Avoid During Pneumonia:
- Sugary Snacks and Sodas: High-sugar foods and beverages can weaken the immune system and promote inflammation, so it’s best to limit or avoid them.
- Processed and Fried Foods: Foods high in salt and saturated fats can exacerbate inflammation and should be minimized.
- Alcohol: Alcohol can dehydrate the body, weaken the immune system, and interfere with medications, so it’s best to avoid it during pneumonia.
- Caffeine: Caffeine can disrupt sleep patterns and hinder your recovery, so it’s a good idea to limit or avoid caffeinated beverages.
- Dairy (if it worsens mucus production): In some cases, dairy products can increase mucus production and make breathing more difficult. If you find that dairy worsens your symptoms, consider limiting your intake.
- Spicy or Acidic Foods: Spicy foods and acidic ingredients, like citrus fruits and tomatoes, can irritate the throat and worsen coughing. If you find these foods uncomfortable, it’s best to avoid them temporarily.
Remember that individual reactions to certain foods can vary. It’s important to listen to your body and adapt your diet based on your specific symptoms and preferences. Consulting with a healthcare professional or a registered dietitian can provide personalized guidance to support your recovery from pneumonia.
Comparison with Other Conditions
Tuberculosis vs. Pneumonia:
- Tuberculosis (TB) is a specific infectious disease caused by Mycobacterium tuberculosis, and it primarily affects the lungs. It’s characterized by a chronic cough, weight loss, and night sweats.
- Pneumonia is a more general term for lung inflammation and infection, often caused by various bacteria, viruses, or fungi. Symptoms include cough, fever, and breathing difficulties.
ARDS vs. Pneumonia:
- Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition that can be caused by various factors, such as pneumonia, sepsis, or trauma. It results in widespread inflammation in the lungs and severe breathing difficulties.
- Pneumonia is one of the potential causes of ARDS. It is a common condition that can lead to lung inflammation and pneumonia symptoms, but ARDS represents a more severe and life-threatening stage of lung dysfunction.
Common Cold Differs from Pneumonia:
- The common cold and pneumonia are both respiratory conditions, but they differ in several ways. The common cold is typically caused by various viruses (e.g., rhinoviruses) and leads to symptoms like a runny or stuffy nose, sneezing, sore throat, and mild fatigue. It is usually a milder and self-limiting illness.
- Pneumonia, on the other hand, is often caused by bacteria, viruses, or fungi and results in lung inflammation. It leads to symptoms like high fever, cough with phlegm, and difficulty breathing. Pneumonia is generally more severe and can be life-threatening, especially in vulnerable populations.
Special Cases and Considerations:
Congenital Pneumonia : Congenital pneumonia is a type of pneumonia that affects newborns or infants within the first few weeks of life. It can be caused by various factors, including infections acquired from the mother during birth, aspiration of amniotic fluid or meconium, or structural lung abnormalities. Prompt medical attention is crucial, and treatment may involve antibiotics and supportive care.
Reasons for Recurrent Pneumonia : Recurrent pneumonia can be caused by multiple factors, including underlying medical conditions, weakened immune system, or lifestyle choices.Common causes include chronic lung diseases (e.g., COPD), immunodeficiency disorders, aspiration (e.g., due to swallowing problems), and smoking. Identifying and addressing the underlying cause is essential to prevent further recurrences.
Pneumonia in Old Age Treatment : Treating pneumonia in older adults may require special considerations due to their often weaker immune systems and higher risk of complications. Treatment involves antibiotics to target the specific causative agent and supportive care, including oxygen therapy and fluids. Hospitalization may be necessary for severe cases. Prevention through vaccination (e.g., pneumococcal and influenza vaccines) is also important for older individuals.
Pneumonia Detection Using Deep Learning:
Advances in medical technology have paved the way for the development of deep learning models for the early detection and diagnosis of pneumonia. These models leverage medical imaging techniques like chest X-rays and CT scans to provide faster and more accurate diagnoses. These AI-based systems offer several advantages:
- Speed: Deep learning models can analyze medical images quickly, allowing for faster diagnosis and treatment planning.
- Accuracy: They can detect subtle abnormalities that may be missed by human radiologists, potentially leading to earlier intervention.
- Consistency: AI models provide consistent results, reducing the potential for human error and variability in interpretations.
- Efficiency: They can assist healthcare professionals by triaging cases, helping prioritize urgent cases, and streamlining the diagnostic process.
- Access: AI-based pneumonia detection can be valuable in regions with limited access to expert radiologists, enabling broader access to quality healthcare.
Understanding the types and classifications of pneumonia is crucial for accurate diagnosis and effective treatment. Pneumonia can result from various pathogens, impacting distinct lung regions, and can be contracted in diverse environments. Recognizing these distinctions is vital for healthcare professionals to provide the best care for patients. Whether it’s bacterial or viral, lobar or bronchopneumonia, or community-acquired or hospital-acquired, proper classification helps guide the treatment approach and improve patient outcomes.
Frequently Asked Questions:
- What are the typical symptoms of pneumonia?
Symptoms may include a persistent cough, chest pain, shortness of breath, fever, and fatigue. Severity can vary, and it’s essential to seek medical attention if symptoms worsen or persist. - Can pneumonia be prevented?
Yes, practicing good hygiene, getting vaccinated against relevant pathogens, and avoiding exposure to known risk factors can help prevent pneumonia. It’s crucial, especially for vulnerable populations, like the elderly or those with weakened immune systems. - Are intravenous antibiotics always necessary for pneumonia treatment?
Intravenous antibiotics are typically recommended for severe or bacterial pneumonia cases. The choice of antibiotics depends on the specific bacteria causing the infection and the patient’s overall health. Always follow your doctor’s advice regarding antibiotic treatment. - How can I manage symptoms of usual interstitial pneumonia at home?
While there is no cure, symptom management includes staying active within limits, maintaining a healthy lifestyle, and following prescribed medications. Regular follow-ups with healthcare providers are crucial. - Is oxygen therapy necessary for UIP patients?
Oxygen therapy may be recommended if lung function is significantly impaired. It helps improve oxygen levels in the blood and reduces breathlessness. Your healthcare team will determine the appropriate level of oxygen support. - How is usual interstitial pneumonia diagnosed?
Diagnosis involves a combination of clinical history, imaging studies like high-resolution CT scans, and sometimes a lung biopsy to confirm the presence of characteristic patterns
References:
- Pneumonia https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/
- Types and Classifications https://my.clevelandclinic.org/health/diseases/4471-pneumonia
- Identifying Specific Bacteria and Organisms https://www.ncbi.nlm.nih.gov/books/NBK525768/
- Post-COVID Pneumonia and Complications https://my.clevelandclinic.org/health/diseases/24002-covid-pneumonia
- Diet and Nutrition During Pneumonia https://www.lybrate.com/topic/diet-for-pneumonia
- Pneumonia Detection Using Deep Learning https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9356824/
About Author –
Dr. Gopi Krishna Yedlapati, Consultant interventional pulmonologist, Yashoda Hospital, Hyderabad
MD, FCCP, FAPSR (Pulmonology)












 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More