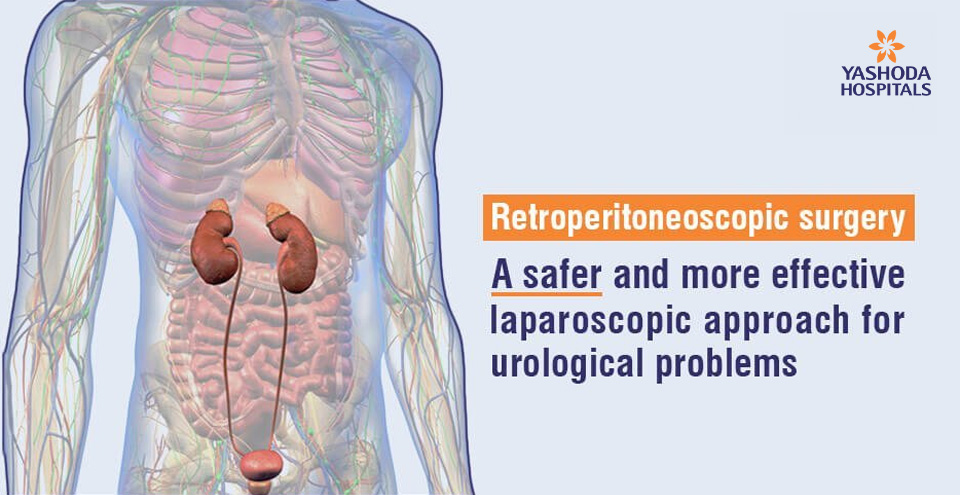
Retroperitoneoscopic surgery for urological diseases
At a Glance:
1. What is retroperitoneoscopic surgery?
2. What are the indications of retroperitoneoscopic surgery?
3. What are the contraindications of retroperitoneoscopic surgery?
4. What to expect before retroperitoneoscopic surgery?
5. How is retroperitoneoscopic surgery performed?
6. What are the advantages of retroperitoneoscopic surgery?
7. Is retroperitoneoscopic surgery safe, are there any risks?
8. How should one choose a facility for retroperitoneoscopic surgery?
What is retroperitoneoscopic surgery?
Retroperitoneoscopic surgery is an advanced, minimally invasive surgery for the treatment of certain conditions of the renal or the urinary system. Laparoscopic surgery for many of the renal conditions is performed using two approaches namely transperitoneal and retroperitoneal.
The organs within the abdomen such as the liver and intestines are covered by a membrane called the peritoneum and the area outside or behind the peritoneum is called retroperitoneum. The anatomical structures and organs behind the peritoneum are called ‘retroperitoneal’. Some of the retroperitoneal organs are the adrenal glands, kidneys, ureter, the abdominal aorta, inferior vena cava, and their branches.
In retroperitoneoscopic surgery, the procedure is performed via laparoscopic ports, usually three or four in number, that are inserted in a person’s flank region away from the abdomen. The operating surgeon can visualize and operate on the organs present in the retroperitoneum when indicated through these ports.
The first retroperitoneoscopic surgery was performed by Prof. Wickham in 1979 for the removal of a ureteric stone. It became a viable alternative to the transperitoneal approach after Prof. Ralph Clayman and later Dr. Gaur modified it further by using a balloon to distend the retroperitoneal space (RPS) before pneumo-insufflation was done. The technique is now popular and widely practiced worldwide by urosurgeons.

What are the indications of retroperitoneoscopic surgery?
Amongst the various procedures that are performed in urology, the following surgeries related to kidneys, adrenal gland and ureter are can be done using the retroperitoneoscopic approach:
- Simple nephrectomy due to stones and/or ureteropelvic junction obstructions (UPJOs)
- Partial nephrectomy for kidney tumors
- Radical nephrectomy for kidney tumors
- Donor nephrectomy (both sides)
- Adrenalectomy up to 7-8 cms of adrenal masses
- Ureterolithotomy for large ureteric stones not amenable to endoscopic surgery
- Nephropexy: surgical fixation of a floating or mobile kidney
- Renal biopsy
- Renal cyst marsupialization to remove a cyst and create a new surface
- Retroperitoneal lymph node dissection
- Stones in the ureter, not amenable to treatment by endourological procedures.
- Ureterocutaneostomyfor incontinence
- Ureterolysis to expose or free the ureter from any kind of blockage or external pressure
Retroperitoneoscopic nephrectomy: Nephrectomy of benign renal disorders has been one of the most commonly performed retroperitoneoscopic procedure. Conditions like long standing hydronephrosis due to UPJO or stone disease, reflux nephropathy, etc can lead to nonfunctioning kidney requiring ablation of the unit which can be done with this approach.
Retroperitoneoscopic adrenalectomy: A retroperitoneoscopic adrenalectomy (RPA) can be performed for persons who require unilateral or bilateral adrenalectomies for benign tumors or isolated metastases, and who are not candidates for a transabdominal laparoscopic procedure. RPA is technically challenging hence it requires specific training and expertise for a surgeon to perform this procedure.
What are the contraindications of retroperitoneoscopic surgery?
Retroperitoneoscopic surgery is safe and feasible for many urological procedures. However, people with certain conditions are considered to be unfit for laparoscopic procedures and they are an absolute contraindication for retroperitoneoscopic surgery too. Some of these contraindications are:
Previous open surgery in retroperitoneum. PCNL itself is not a contraindication for this approach.
- Uncorrected coagulopathy
- Retroperitoneal fibrosis
- Significant ileus or bowel obstruction
- Severe cardiac or pulmonary diseases.
- Gross skeletal abnormalities like extensive kyphosis or scoliosis.
What to expect before retroperitoneoscopic surgery?
To ensure optimized patient outcomes, accurate diagnosis of the condition for which retroperitoneoscopic surgery is indicated is essential. Perioperative evaluation of the person is done by the doctors based on the following investigations and information:
Clinical history and physical examination: During the initial consultation with the surgeon, he or she will review the person’s medical history and advice relevant investigations.
A brief physical examination will be performed at the time of the consultation. If the surgeon determines that the person is a suitable candidate for surgery, he or she may be explained the procedure to be followed before the surgery.
Before the procedure: The doctor would advise specific preparatory instructions depending on the person’s medical status. Some of the commonly advised preparatory instructions are as follows:
- Pre-anesthetic checkup to determine fitness for anesthesia
- A soft diet for a day or two days before the procedure.
- The doctor’s instructions regarding any prescription medication that a person may be on should be adhered to. For example, if a person is on an anticoagulant or antiplatelet medication, he/she may be advised to stop it before the procedure.
- The person may be placed on antibiotics before the procedure.
- Any allergies should be disclosed to the treating doctor during the medical history.
How is retroperitoneoscopic surgery performed?
Posterior retroperitoneoscopic surgery is performed under general anesthesia. The technique requires the person to be operated to lie in lateral position on the operating table. In this procedure, the retroperitoneal space is directly approached from the flank.
- A series of small incisions are made from the lower border of the tip of the 12th rib.
- Access to the retroperitoneal space is achieved through these incisions by splitting the muscle under direct vision. A saline inflated balloon in retroperitoneum creates a space. After this the trocars are placed. Trocars used are usually three in number. The trocar functions as a portal for the placement of the surgical instruments and a telescope for a videoscopic view of the surgical site.
- Appropriate suturing is done around the trocar to ensure an airtight seal.
- A telescope measuring 5- or 10-mm is inserted through the first trocar.
- The second trocar measuring approximately 3-mm is inserted near the costovertebral angle i.e. the angle formed at the side of the back between the twelfth rib and the vertebral column.
- The third trocar measuring approximately 3-mm is inserted above the top of the iliac crest that is close to the surface of the skin in the hip region and the anterior axillary line.
- The laparoscope and the operating instruments are inserted through the ports and the surgical procedure is carried out.
What are the advantages of retroperitoneoscopic surgery?
The organs present in the peritoneal cavity do not stick to each other due to a lubricious fluid present in this membrane. Entering the abdomen during an operation with the transperitoneal approach can damage this balance in the peritoneum which may result in the sticking of organs to each other. Retroperitoneoscopic surgery, on the other hand, has the distinct advantage of direct access to the retroperitoneal organs. As a result, an entry in the peritoneal cavity is avoided, thereby preventing the risk of adhesive obstructions of the intestine. Many studies have demonstrated superior outcomes in surgeries done with the retroperitoneoscopic approach in comparison to the traditional laparoscopic procedure through the abdomen.
Some of the advantages of retroperitoneoscopic approach for the patients include:
- Less operating time
- Minimal blood loss during surgery
- Cosmetic superiority due to less scarring and scar location below the undergarment line
- Less post-operative pain
- Quicker recovery and return to normal activities
- A shorter stay in the hospital
- Safety
- Prevention of gas formation and bloating in the intestines
Some of the benefits experienced by the operating surgeons include:
- Avoidance of damage to the peritoneal membrane and the intra-abdominal organs during surgery
- Reduced risk of repeat surgery due to intra-abdominal adhesions
- Prevention of other associated complications like uterine adhesions in women that would pose a risk for childbearing
- Reduced risk of herniation in the surgical access site
- Prevention of spillage of infected urine into the peritoneal cavity.
Despite the distinct advantages of the approach, there are some constraints like limited working space for dissection so larger pathologies like hydronephrotic kidneys or large renal tumors may not be amenable to treatment with a retroperitoneoscopic approach.
Is retroperitoneoscopic surgery safe, are there any risks?
Retroperitoneoscopic surgery is a safe and feasible option when performed by well-trained and experienced surgeons. As mentioned earlier, the risk of damage to the peritoneal membrane is greatly reduced thereby eliminating the risk of accidental injury and adhesion of the delicate intra-abdominal organs.
Even though it is considered a safe procedure, it is not devoid of certain risks. These risks include general risks as well as some procedure-specific risks like:
- Bleeding and infection from the site of surgery
- Collateral damage to the nearby structures like soft tissues, nerves or blood vessels
- Side effects of anesthesia that may include:
- Drowsiness
- Headache
- Heart attack or stroke in extremely rare cases
- Nausea
- Sore throat, due to the breathing tube if used during surgery
- Death are extremely rare.
Procedure specific risks: Similar to other newer and novel techniques, retroperitoneoscopic surgery too has witnessed a certain learning curve. Scientific studies by some urological associations have estimated the overall complication rate to be 4.9%. The complication rate gets affected by the difficulty of the procedure. In general, the complications that occur after retroperitoneoscopic surgery are relatively mild and easy to be managed expectantly and medically. Some of the commonly encountered complications are:
- Hemorrhage
- Dense adhesions requiring open surgical conversion
- Wound infection.
- Distortion of anatomy for urologists not exposed to this procedure
- Pneumothorax consequent to CO2 insufflation
Some complications which may be encountered during other laparoscopic procedures may well be relevant to retroperitoneoscopic procedures too. These include:
- Subcutaneous emphysema: An abnormal collection of gas or air in the layer under the skin
- Pneumomediastinum: An abnormal collection of gas or air in the mediastinum, the center of the chest in between the lungs.
How should one choose a facility for retroperitoneoscopic surgery?
Considering the need for sophisticated equipment, infrastructure, and considerable surgical expertise, retroperitoneoscopic surgery is recommended to be performed in high volume, specialized centers. This ensures the procedure is matched with the correct indications. Long term follows up to evaluate the performance and follow-up of newer techniques is also a well-coordinated activity in such centers. Retroperitoneoscopic technique requires experience and attention for performing the surgery in a narrow area. This is one of the primary reasons that it is not performed commonly in all centers. Very few urologists are trained in retroperitoneoscopy.
The Institute of Urology at Yashoda Hospitals is a high-volume tertiary referral center for uro- surgeries. Our expert uro-surgeon has experience of more than 1500 procedures in last 15 years and frequently treats patient who are turned away by less experienced centers as being too risky or complex to operate on. Our surgeons also operate persons with rare tumors and syndromes who may require extensive diagnostic work-up.
State-of-the-Art Procedures: We at Yashoda hospital offer patients complex procedures such as RPN (retroperitoneoscopic nephrectomy). The multidisciplinary uro surgery, transplantation experts and other specialist teams of oncology, endocrinology, etc at Yashoda hospital provide seamless expert care in diagnosing and treating patients with different urological conditions.
Conclusion:
Retroperitoneoscopic surgery enables minimally invasive treatment for many urological and nephrological conditions. The major advantage associated with the retroperitoneoscopic approach is reduced surgical trauma, significant reduction of post-operative pain, a shorter period of stay in hospital and faster recovery. In addition to this, there is a better cosmetic result.
The operating time is usually dependent on the type of pathology and the surgeon’s expertise. Many urological procedures are currently carried out laparoscopically via the retroperitoneal approach which has become the technique of choice at an increasing number of specialized centers for several indications, that may include simple nephrectomy, living donor nephrectomy, partial or radical nephrectomy, and nephroureterectomy and adrenalectomy to name a few.
There is evidence from many studies to believe that retroperitoneal laparoscopy (RPL) can prove to be advantageous over transperitoneal laparoscopy due to its advantages like safe port placement, lesser risk of injury to abdominal organs, etc. However, retroperitoneoscopic surgery can be technically more challenging because of the smaller working space thereby calling for considerable surgical expertise in performing this procedure.
References:
- European Association of Urology. Retroperitoneoscopy: A Versatile Access for Many Urologic Dogu Teber, Ahmet Tefekli. Available at:https://www.eusupplements.europeanurology.com/article/S1569-9056(06)00235-1/pdf. Accessed on November 29, 2019
- Bombay Hospital Journal.The Evolution Of Retroperitoneal Laparoscopy, Durga D Gaur, Available at.https://www.bhj.org.in/journal/2002_4402_apr/endo_142.htm. Accessed on November 29, 2019
- Journal of Urology. Retroperitoneoscopy: Experience With 200 Cases Jens J. Rassweiler. Available at: https://www.auajournals.org/doi/abs/10.1016/S0022-5347%2801%2962512-6. Accessed on November 29, 2019















 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More