Preventive Care in Gastroenterology
1. Preventive Care in Gastroenterology
2. Understanding the Prevalence of Gastrointestinal and Liver Issues
3. Digestive Health: Navigating IBD, Glycemic Index Cancers, Gallbladder, and Pancreatitis
4. Non-Surgical Approaches and Laser Treatments for Liver, Gallbladder, & Pancreas Health
5. Diagnostic Technologies in Gastroenterology
6. Lifestyle Impact in Gastroenterology
7. Preventive Tips for Gallstone, GERD, and Liver & Pancreas Wellness
Gastroenterology, a branch of medicine focused on the digestive system, has witnessed remarkable advancements in preventive care and endoscopic procedures. These innovations not only contribute to the early detection of gastrointestinal disorders but also enhance the efficacy of treatments. Let’s delve deep into the importance of preventive care in gastroenterology and explore the latest advances in endoscopic procedures, including advanced endoscopy, various types of endoscopy, and the role of surgical endoscopy.
Preventive Care in Gastroenterology:
Preventive care is a cornerstone of gastroenterology, aimed at identifying and addressing potential health issues before they escalate. Key components of preventive care in gastroenterology include regular screenings, lifestyle modifications, and vaccination against certain infections. By adopting a proactive approach, individuals can reduce the risk of developing severe gastrointestinal conditions such as colorectal cancer, inflammatory bowel disease, and liver diseases.
Advanced Endoscopy: Advanced endoscopy plays a pivotal role in the diagnosis and treatment of gastrointestinal disorders. Here are some notable advancements in this field:
- High-Resolution Endoscopy: High-resolution endoscopy involves the use of advanced imaging technologies which enables gastroenterologists to visualize subtle abnormalities and lesions that might be missed with traditional endoscopy. The improved clarity aids in early detection and precise diagnosis.
- Chromoendoscopy: Chromoendoscopy involves the application of special dyes or stains during endoscopy to enhance the visualization of abnormalities in the gastrointestinal tract. This technique is particularly useful in detecting early signs of dysplasia in conditions like inflammatory bowel disease and Barrett’s esophagus.

Types of Endoscopy: Different types of endoscopic procedures are tailored to examine specific parts of the digestive system. Here are some common types:
- Esophagogastroduodenoscopy (EGD): EGD is a procedure used to examine the lining of the esophagus, stomach, and duodenum. It is valuable for diagnosing conditions such as ulcers, inflammation, and tumors. Advanced technologies, such as capsule endoscopy, have further improved the visualization of the upper gastrointestinal tract.
- Colonoscopy: Colonoscopy is a crucial screening tool for colorectal cancer. Recent advancements include virtual colonoscopy, which uses computed tomography (CT) scans to create detailed images of the colon, providing an alternative to traditional colonoscopy.
- Endoscopic Ultrasound (EUS): EUS combines endoscopy with ultrasound technology to obtain detailed images of the digestive tract and adjacent structures. This procedure is particularly useful for staging cancers, evaluating pancreatic disorders, and obtaining biopsies.
Surgical Endoscopy: Surgical endoscopy involves using endoscopic techniques for therapeutic interventions. Here are some key aspects:
- Endoscopic Mucosal Resection (EMR): EMR is a minimally invasive procedure used to remove abnormal tissues or early-stage cancers from the digestive tract lining. This technique helps avoid more extensive surgeries, promoting quicker recovery.
- Endoscopic Submucosal Dissection (ESD): ESD is an advanced technique for the removal of larger lesions or early-stage cancers in the gastrointestinal tract. It allows for en-bloc resection of tumors, reducing the need for surgery and preserving organ function.
Understanding the Prevalence of Gastrointestinal and Liver Issues
What Causes Gastric Problems:
- Dietary Factors: Consuming spicy, greasy, or acidic foods can contribute to gastric problems.
- Infections: Bacterial or viral infections affecting the stomach and intestines can lead to gastric issues.
- Chronic Conditions: Conditions like gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), and inflammatory bowel diseases (IBD) can cause ongoing gastric problems.
- Medications: Some medications, especially non-steroidal anti-inflammatory drugs (NSAIDs), can irritate the stomach lining.
- Stress: Emotional stress can exacerbate gastric symptoms.
- Smoking and Alcohol: Both can contribute to gastric issues and should be moderated.
1.Gastrointestinal and Liver Issues: Liver Acidity: Liver acidity, although not a medical term, may refer to symptoms related to acid reflux or indigestion. It’s important to note that the liver itself doesn’t produce acid, but gastrointestinal issues can manifest with symptoms that might be perceived as acidity. Common symptoms include:
- Heartburn (Chest burning post-meals from stomach acid in the esophagus.)
- Indigestion (Upper abdominal discomfort, bloating, fullness.)
- Regurgitation (Stomach contents, acid returning to the mouth.)
- Nausea (Queasiness, urge to vomit.)
- Bitter Taste (Acid reflux may cause a sour or bitter mouth taste.)
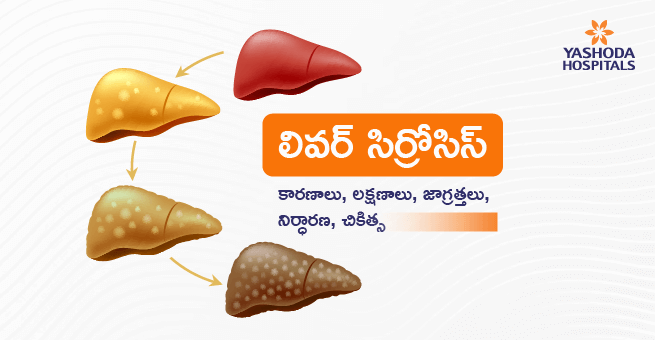
2.Fatty Liver: Fatty liver disease is a condition where fat accumulates in liver cells. It can be caused by excessive alcohol consumption (alcoholic fatty liver disease) or non-alcoholic factors (non-alcoholic fatty liver disease or NAFLD). Common symptoms include:
- Fatigue
- Abdominal discomfort or pain in the upper right side
- Enlarged liver
3.Gallstones: Gallstones are solid particles that form in the gallbladder, often composed of cholesterol or bilirubin. Symptoms may include:
- Abdominal pain, particularly in the upper right abdomen
- Nausea and vomiting
- Jaundice (yellowing of the skin and eyes)
Stomach-Related Problems:
- Gastritis: Inflammation of the stomach lining, often causing stomach pain, nausea, and vomiting.
- Peptic Ulcers: Open sores that develop on the inner lining of the stomach, small intestine, or esophagus, leading to abdominal pain.
- Gastroenteritis: Inflammation of the stomach and intestines, commonly caused by infections, resulting in diarrhea, abdominal cramps, and vomiting.
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux that can cause heartburn and lead to complications if untreated.
- Inflammatory Bowel Disease (IBD): Chronic inflammatory conditions like Crohn’s disease and ulcerative colitis affecting the gastrointestinal tract.
Spotting symptoms like persistent abdominal pain, unexplained weight loss, or discomfort?
Digestive Health: Navigating IBD, Glycemic Index Cancers, Gallbladder, and Pancreatitis
Inflammatory Bowel Disease (IBD):
- IBD encompasses a group of inflammatory conditions affecting the digestive tract, with Crohn’s disease and ulcerative colitis being the most common.
- Symptoms include abdominal pain, diarrhea, weight loss, and fatigue. While the exact cause remains unknown, a combination of genetic, environmental, and immune system factors is believed to contribute.
- Diagnosis involves a thorough medical history, physical examination, and various tests such as blood tests, endoscopy, and imaging studies.
- Treatment may include medications to reduce inflammation, lifestyle changes, and in severe cases, surgery to remove damaged portions of the digestive tract.
Glycemic Index Cancers:
- High glycemic index (GI) diets, spiking blood glucose rapidly, correlate with elevated cancer risks due to inflammation and insulin resistance.
- Opting for a low-GI diet with whole grains and fruits is advised to mitigate this risk.
- Symptoms include weight loss and fatigue, diagnosed through assessing dietary patterns and glucose levels.
- Prevention involves a low-GI diet and lifestyle changes, while treatment options depend on cancer type and stage, encompassing surgery, chemotherapy, or radiation therapy.
Gallbladder Issues:
- The gallbladder, a small organ beneath the liver, plays a crucial role in digestion by storing bile produced by the liver. Gallstones, formed when the balance of substances that constitute bile is disrupted, can lead to complications such as inflammation and infection.
- Symptoms include abdominal pain, nausea, and vomiting.
- Diagnostic tools like ultrasound and blood tests aid in identifying gallbladder issues.
- Treatment options range from dietary changes to surgical removal of the gallbladder, depending on the severity of the condition.
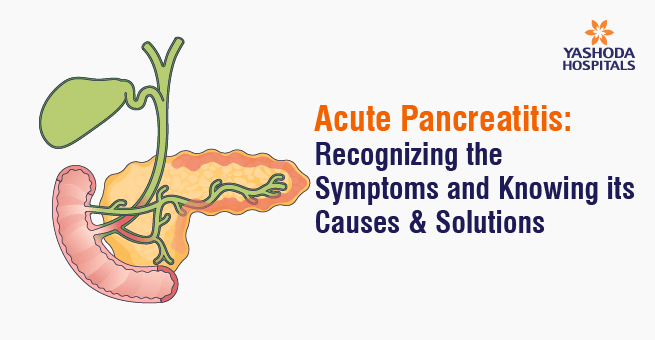
Pancreatitis:
- Pancreatitis, inflammation of the pancreas, can result from gallstones, alcohol consumption, or certain medications.
- Symptoms include abdominal pain, nausea, and fever. Chronic pancreatitis can lead to digestive issues and diabetes.
- Diagnosis involves blood tests, imaging studies, and sometimes a pancreatic function test.
- Treatment includes pain management, lifestyle modifications, and addressing the underlying cause. Severe cases may require hospitalization and nutritional support.
Non-Surgical Approaches and Laser Treatments for Liver, Gallbladder, and Pancreas Health
Treatment without Surgery: Non-surgical treatments for liver, gallbladder, and pancreas issues may include medications, lifestyle modifications, and dietary changes. Conditions such as fatty liver disease might be managed through weight loss, exercise, and medication. Pancreatitis may require enzyme supplements and a low-fat diet, while gallstones could be treated with medications to dissolve them.
Removal without Surgery: Certain conditions, like gallstones, can be addressed without surgery. Gallstone dissolution medications may be prescribed to break down stones. However, this approach depends on the size and type of stones. In some cases, non-surgical removal techniques, such as shock wave lithotripsy, may be considered for gallstones.
Laser Treatment: Laser treatments are often used in pancreas and liver conditions. In pancreatitis, laser therapy might be employed to remove blockages or tumors through endoscopic procedures. In liver conditions, laser therapy may be used to destroy tumors or treat certain liver disorders through minimally invasive techniques.
Signs You Need Treatment: Signs indicating the need for liver, gallbladder, or pancreas treatment include abdominal pain, jaundice (yellowing of the skin and eyes), persistent digestive issues, unexplained weight loss, and changes in urine or stool color. If experiencing severe symptoms or signs of acute conditions like pancreatitis, seeking immediate medical attention is crucial.
It’s important to note that specific treatment approaches depend on the diagnosed condition, and consulting a healthcare professional is essential for accurate diagnosis and tailored treatment plans.
Diagnostic Technologies in Gastroenterology
Diagnostic technology has played a significant role in advancing the field of gastroenterology, enabling more accurate and efficient detection, monitoring, and treatment of gastrointestinal (GI) disorders. Additionally, the impact of diagnostic technology on lifestyle in gastroenterology extends beyond the clinical setting to patient management and overall well-being.
1.Endoscopy:
- Impact: Endoscopy allows direct visualization of the GI tract, aiding in the diagnosis and treatment of conditions such as inflammatory bowel disease (IBD), colorectal cancer, and gastroesophageal reflux disease (GERD).
- Lifestyle Impact: Advanced endoscopic techniques, such as capsule endoscopy, reduce the invasiveness of procedures, leading to shorter recovery times and improved patient comfort.
2.Imaging Modalities:
- Impact: Modalities like CT scans, MRI, and ultrasound provide detailed images of the GI tract, helping in the diagnosis of diseases such as liver cirrhosis, pancreatic disorders, and abdominal tumors.
- Lifestyle Impact: Non-invasive imaging methods contribute to early disease detection, enabling timely intervention and potentially minimizing the impact on daily life.
3.Biomarker Testing:
- Impact: Biomarkers, such as fecal occult blood and C-reactive protein, assist in diagnosing and monitoring conditions like colorectal cancer and IBD.
- Lifestyle Impact: Regular monitoring through non-invasive tests can lead to early detection of relapses or complications, allowing for prompt adjustments in treatment plans.
4.Genetic Testing:
- Impact: Genetic testing aids in identifying hereditary factors contributing to GI disorders, allowing for personalized treatment plans.
- Lifestyle Impact: Knowledge of genetic predispositions can influence lifestyle choices and screening frequencies, enhancing preventive measures for those at higher risk.
Lifestyle Impact in Gastroenterology
Lifestyle modifications play a crucial role in managing and potentially curing certain gastrointestinal conditions, including gastroesophageal reflux disease (GERD), improper digestion, esophageal ulcer symptoms, and food pipe ulcers. Here are some lifestyle impacts and recommendations for these conditions:
Gastroesophageal Reflux Disease (GERD):

1.Dietary Modifications:
- Certain foods and beverages can trigger acid reflux. Avoiding acidic, spicy, and fatty foods, along with minimizing alcohol and caffeine intake, can alleviate GERD symptoms.
- Adopting a GERD-friendly diet can contribute to long-term symptom relief and healing of the esophagus.
2.Weight Control:
- Excess weight can contribute to increased pressure on the stomach, leading to acid reflux. Weight loss can alleviate symptoms and improve overall health.
- Maintaining a healthy weight through proper diet and exercise can be instrumental in managing and potentially curing GERD.
3.Bed Elevation:
- Elevating the upper body during sleep can help prevent stomach acid from flowing into the esophagus.
- Adjusting sleeping habits, such as using a wedge pillow or raising the bed, can provide relief and contribute to long-term management.
4.Meal Timing:
- Eating smaller, more frequent meals and avoiding late-night snacks can reduce the likelihood of acid reflux.
- Adapting meal habits can positively impact digestion and prevent GERD symptoms.
Improper Digestion:
- Chewing Practices:
- Proper chewing aids in the initial stages of digestion. Inadequate chewing can lead to difficulty in breaking down food.
- Cultivating mindful eating habits can promote better digestion and nutrient absorption.
- Hydration:
- Insufficient water intake can hinder digestion. Water helps break down food and move it through the digestive tract.
- Ensuring adequate hydration supports optimal digestion and can alleviate symptoms of improper digestion.
Esophageal Ulcer Symptoms and Food Pipe Ulcers:
- Avoiding Irritants:
- Certain substances, such as tobacco and certain medications, can irritate the esophagus and contribute to ulcer formation.
- Eliminating or reducing exposure to these irritants can support the healing of esophageal ulcers.
- Medication Adherence:
- Following prescribed medications, such as proton pump inhibitors (PPIs) or H2 blockers, can help reduce stomach acid and promote ulcer healing.
- Consistent medication adherence is crucial for managing and treating esophageal ulcers.
- Stress Management:
- Stress can exacerbate symptoms and delay the healing of ulcers.
- Incorporating stress-reducing activities, such as meditation or exercise, can support the overall healing process.
While lifestyle modifications can significantly improve symptoms and contribute to the management of these conditions, it’s important to note that consulting with a healthcare professional is essential for a comprehensive and personalized treatment plan. Individual responses to lifestyle changes may vary, and medical guidance is crucial for addressing specific health concerns.
Preventive Tips for Gallstone, GERD, and Liver & Pancreas Wellness
Preventing Gallstones:
- Balanced Diet: Include fruits, vegetables, and whole grains; limit saturated fats.
- Hydration: Drink enough water to prevent gallstone formation.
- Exercise: Stay active to maintain a healthy weight.
- Gradual Weight Loss: Aim for a steady weight loss process.
Preventing GERD:
- Maintain a Healthy Weight: Adopt a healthy diet and exercise regularly.
- Dietary Changes: Avoid trigger foods and eat smaller, more frequent meals.
- Elevate the Head of the Bed: Reduce nighttime reflux by raising the bed.
Vaccination for Liver Health:
- Hepatitis A and B Vaccines: Guard against hepatitis viruses.
- HPV Vaccine: Reduce the risk of liver cancer.
Early Identification and Intervention:
- Regular Check-ups: Schedule routine check-ups for digestive health.
- Know the Symptoms: Be aware of gallstone, GERD, liver, and pancreas issue symptoms.
- Screening Tests: Discuss screening tests with your healthcare provider based on risk factors.
Lifestyle Choices: Diet, Exercise, Smoking, and Alcohol

Diet and Exercise: Our lifestyle choices significantly impact overall health, particularly regarding conditions like GERD, gallstones, and pancreatic health. A balanced diet, rich in nutrients and mindful of triggers, along with regular exercise, supports digestive well-being. Smaller, frequent meals alleviate GERD symptoms, while a low-fat diet and exercise aid in weight management and prevent gallstones.
Smoking and Alcohol: Quitting smoking, moderating alcohol intake, or abstaining altogether, is vital for digestive health. Adopting these lifestyle practices establishes a foundation for overall well-being. Always consult healthcare professionals for personalized advice.
Gastrointestinal and liver issues encompass a wide spectrum of conditions with varying causes and symptoms. Recognizing the signs, understanding the underlying factors, and seeking timely medical attention are crucial for effective management and maintaining digestive health. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can play a significant role in preventing and managing these issues.
Frequently Asked Questions:
What are some common digestive disorders?
Common digestive disorders include gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), celiac disease, and gallstones. Gastroenterologists diagnose and treat these conditions through various medical and procedural interventions.
How can I maintain a healthy digestive system?
Maintaining a healthy digestive system involves adopting a balanced diet rich in fiber, staying hydrated, practicing portion control, exercising regularly, and avoiding excessive alcohol and tobacco use. Regular check-ups with a gastroenterologist can also help detect and address potential issues early.
Can diet affect digestive health?
Yes, diet plays a significant role in digestive health. Consuming a diet high in fiber, fruits, vegetables, and whole grains can promote regular bowel movements and support a healthy digestive system. Gastroenterologists often provide dietary recommendations tailored to specific digestive conditions.
How to cure GERD permanently?
There is no guaranteed permanent cure for GERD. However, lifestyle changes, medication, and, in some cases, surgery can effectively manage and alleviate symptoms. Regular consultation with a healthcare professional is essential for personalized treatment.
What is a colonoscopy, and why is it recommended?
A colonoscopy is a procedure that allows a gastroenterologist to examine the inside of the colon and rectum using a flexible tube with a camera. It is commonly recommended for the early detection and prevention of colorectal cancer. During the procedure, polyps, which can potentially develop into cancer, can be removed, reducing the risk of colorectal cancer.
What are the risk factors for liver disease?
Risk factors for liver disease include excessive alcohol consumption, viral hepatitis infections (such as hepatitis B and C), obesity, diabetes, and certain medications. Regular liver function tests and screenings can help identify potential issues early.
References:
- Preventive Care https://journals.lww.com/ajg/fulltext/2017/02000/acg_clinical_guideline__preventive_care_in.15.aspx
- Advanced Endoscopic Procedures https://www.ucsfhealth.org/treatments/advanced-endoscopic-procedures
- Gastroenterology https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7713642/
- Lifestyle Changes https://www.narayanahealth.org/blog/lifestyle-changes-for-gastrointestinal-health-tips-and-strategies-for-prevention
- Gallstones https://www.healthline.com/health/gallstones
About Author –












 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More