Pituitary Gland Tumors – Important Things To Know About
At a glance:
What is the pituitary gland?
The pituitary is the “master gland” that protrudes from the bottom of the hypothalamus in the brain, just behind the eyes. It is a pea-sized gland that works hand-in-hand with hypothalamus to regulate the essential functions of the body.
The pituitary gland controls the other glands and maintains hormonal balance all over the body. This way, the pituitary gland is responsible for growth, development, and reproduction. It also controls the function of the vital organs, such as the kidneys, breasts, and uterus in women.
Without pituitary gland, the water balance, blood pressure, energy balance, temperature regulation, reproductive functions, and metabolism can go haywire. Thus, pituitary gland plays a significant role in helping us lead a healthy life.
What are Pituitary gland tumors or pituitary adenomas?
Pituitary gland tumors are one among the common brain tumors reported in India. Nearly all pituitary adenomas are non-cancerous, abnormal growth in the pituitary gland. They are usually slow-growing and benign, which means they remain localized and do not spread to other parts of the body (benign). On the other hand, pituitary carcinomas (neuroendocrine tumors) are rare, aggressive, cancerous and spread to other parts of the body (malignant).
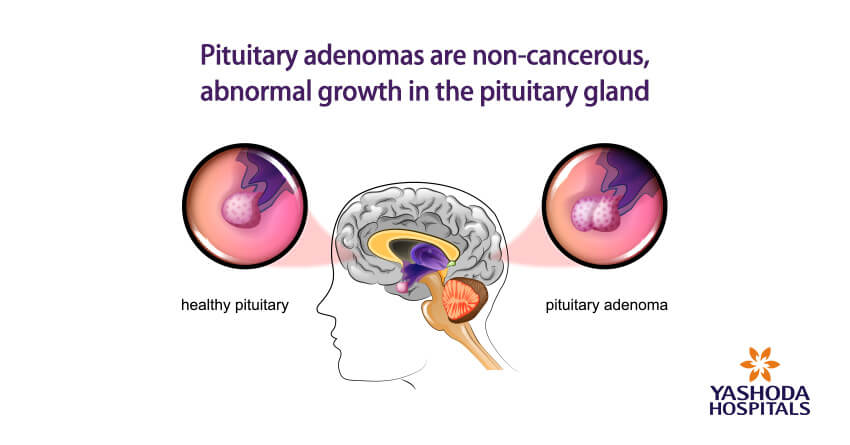
As the pituitary adenomas grow in size, they may compress nearby structures, such as the nerves connecting eyes to the brain. This “mass effect” can result in symptoms related to the organs affected, vision changes as in this case. Large pituitary adenomas (pituitary macroadenomas) can also crush the normal pituitary cells and alter their regulatory activities.
What are the types of pituitary gland tumors?
Based on their influence on hormonal secretions, pituitary adenomas are either functional or nonfunctional:
Functional pituitary adenomas: Pituitary adenomas that release hormones (usually in excess) are called as functional pituitary adenomas. Based on the hormones they secrete and the resulting symptoms, they are further classified as –
- Prolactin-producing tumors (prolactinomas)
- ACTH-producing tumors
- Growth hormone-producing tumors
Non-functional pituitary adenomas do not secrete active hormones. About one-third of the pituitary adenomas are non-functional. They usually grow in size and produce symptoms due to mass effect, leading to a condition called hypopituitarism (diminished hormone secretion by the pituitary gland, causing dwarfism in children and premature aging in adults).
Based on the size of the tumor, pituitary adenomas are called as microadenomas or macroadenomas:
Pituitary microadenomas, tumors smaller than one cm.
Pituitary macroadenomas, tumors larger than one cm.
How do pituitary gland tumors present? What are the symptoms of pituitary adenomas?
Pituitary adenomas show symptoms related to changes in hormone release and mass effect of large tumors on the nearby structures.
Symptoms related to excess hormones:
- Gigantism, Acromegaly (Growth hormone excess): Excessive or very rapid growth (being tall), joint pain, increased sweating, etc.
- Cushing’s syndrome (ACTH excess): Unexplained weight gain, weak bones, reduced libido, high blood sugars, etc.
- Prolactin excess: Prolactin-secreting adenomas can cause infertility, weak bones, and excessive milk secretion in women (galactorrhea) and erectile dysfunction in men.
- Hyperthyroidism (TSH excess): Thyrotropin-secreting adenomas cause symptoms such as rapid or irregular heartbeat, tremors, increased appetite, trouble falling asleep and enlarged thyroid.
Symptoms related to mass effect from pituitary macroadenomas or pituitary carcinomas:
- Vision loss
- Loss of outer peripheral vision
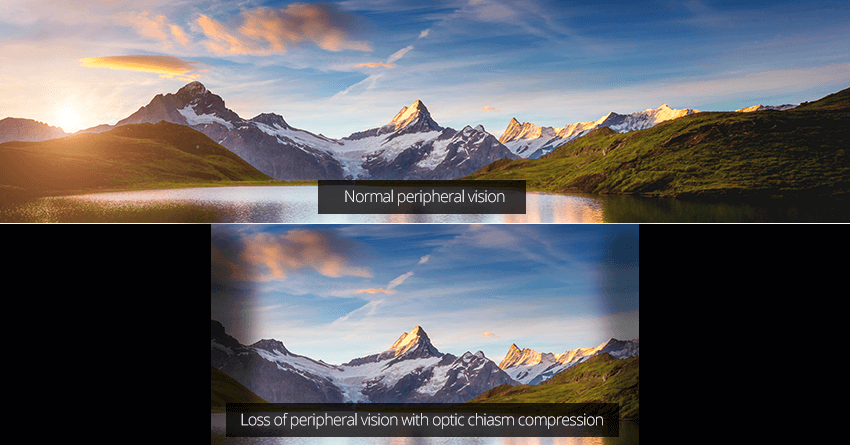
- Blurred vision
- Colors not perceived as bright as usual
- Sudden blindness
- Facial numbness or pain
- Dizziness
- Loss of consciousness
- Loss of pituitary function and decreased release of hormones
- – Reduced sex hormones
- – Hypothyroidism
- – Adrenal insufficiency
- – Low prolactin levels
- – Headache
General symptoms of pituitary adenomas include:
- Headaches,
- Vision problems (double vision, vision loss),
- Nausea or vomiting,
- Behavioral changes, including hostility, depression and anxiety.
What are the causes of pituitary gland tumors?
Pituitary gland tumors are usually spontaneous and not inherited. The exact reason for the tumorous growth is unknown. According to American Cancer Society, there are no causative lifestyle-related or environmental factors for pituitary adenomas.
Pituitary adenomas may occur as a result of genetic mutations caused by exposure to harmful radiations and cancer-causing chemicals.
Who is prone to pituitary gland tumors? What are the risk factors?
There are very few risk factors associated with pituitary gland tumors. Some cases are related to inherited syndromes; however, not everyone having them will have pituitary adenomas.
Family history: Pituitary tumors do not run in families. When found they are also related to other tumors as a part of inherited genetic syndromes.
People with certain inherited syndromes: Genetic mutations and their associated family cancer syndromes include multiple endocrine neoplasias, McCune-Albright syndrome, and Carney complex.
How do pituitary gland tumors progress? What are their complications?
Pituitary adenomas rarely progress to pituitary carcinoma, so there is no staging developed for it. The significant features of pituitary adenomas which help in monitoring the progress of the tumor include:
- Size – microadenoma or macroadenoma
- Growth into nearby structures such as skull
- Symptoms such as vision changes
- Excess hormone release – functional or non-functional
- Type of hormone release affected
Based on the above factors, untreated pituitary adenomas may lead to serious symptoms, complications and comorbidities.
Can pituitary adenomas be detected early?
There are no recommended screening tests to detect pituitary adenomas for people without symptoms or risk factors. Therefore, early detection of pituitary adenomas are rare, and a result of brain scans done for unrelated problems.
Small-sized functional adenomas are easier to detect than the non-functional ones. This is because non-functional adenomas do not cause any symptoms until they grow large enough to press on the nearby tissues.
How do doctors test and diagnose pituitary gland tumors?
Neurologists perform following checks to diagnose pituitary adenomas:
- Medical history
- Physical examination– vision checks, damage to nervous system. You may also have to see an eye specialist.
- Blood and urine tests of hormone levels– endocrinologists and neurosurgeons may recommend several tests to detect hormonal changes and neuronal (related to nerves) changes in the brain.
- Testing for diabetes insipidus
- Venous blood sampling for suspected Corticotroph (ACTH-secreting) adenomas
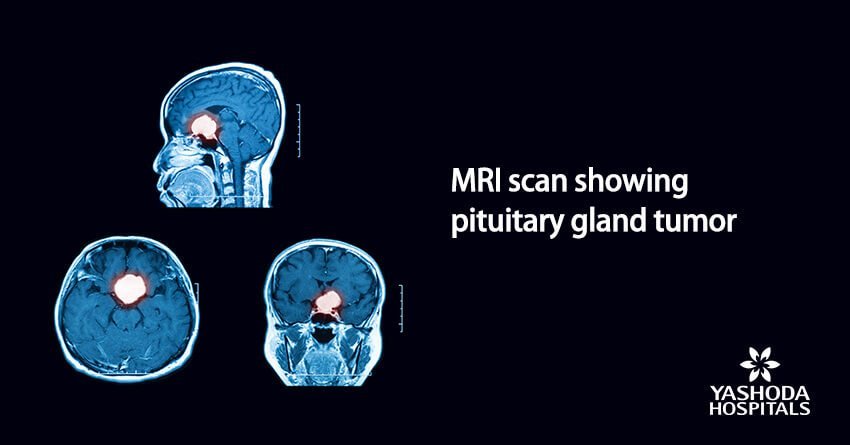
- Imaging tests
- – MRI scans provide detailed images of adenomas larger than 3 mm across.
- – CT scans can find large adenomas, but MRI scans offer better clarity in detecting for brain and pituitary tumors.
- Pituitary tissue biopsy: Doctors perform a biopsy before they can begin treatment. However, if the hormone tests are accurate, you may not need a pituitary tissue biopsy. The doctor will pick a small sample of pituitary tissue for testing under a microscope to confirm the presence of pituitary adenoma cells.
What are the different treatments available for pituitary gland tumors?
For functional pituitary adenomas:
Medicines are often the only treatment needed.
- Dopamine agonists which can stop prolactinomas from making too much prolactin and shrink these tumors. For example, Cabergoline and Bromocriptine are most commonly used to shrink prolactin-secreting adenomas.
- Somatostatin-like medicines such as octreotide, lanreotide are human-made forms of the natural hormone somatostatin. Somatostatin blocks the formation of growth hormone (somatotropin) by growth hormone-secreting adenomas.
For non-functional pituitary adenomas:
- Endoscopic transsphenoidal surgery is the gold standard treatment. The surgeon passes instruments through the nose and opens the sphenoid sinus, reach the pituitary gland and take out the tumor. The transsphenoidal approach has many advantages. No part of the brain is touched during the surgery, so the chance of damaging the brain is limited. There may be fewer side effects, and there’s also no visible scar. Technology in the form of Neuronavigation and Intraoperative MRI imaging has made the surgery a lot safer these days.
- Stereotactic radiosurgery: For microadenomas and residual/recurrent tumors after transsphenoidal surgery, Stereotactic radiosurgery is one good option. In this procedure, the tumor area is destroyed using a large, precise radiation dose. Though this is called radiosurgery, no cutting or surgery is involved. In some cases, the procedure might be done in a few sessions (called stereotactic radiotherapy). Stereotactic radiosurgery targets the tumor more precisely than standard radiation, causing less harm to the normal tissues in the pituitary gland and preventing or reducing radiation exposure to the rest of the brain.
Follow-up care: Once the treatment procedures are complete, doctors want to monitor the recovery for months and years ahead. After surgery, the patient is followed-up by an endocrinologist and a neurosurgeon on a regular basis. It is important to discuss symptoms such as fatigue, gastrointestinal upset, gallstones, and vision problems.
More than 1 million cases of pituitary adenomas are reported in India every year. Although early diagnosis is difficult in many cases, unlike before, pituitary gland tumors are now treatable with medicines and advanced technologies such as stereotactic radiosurgery and endoscopic surgeries. Pituitary adenomas are commonly associated with vision changes and headache. Do not ignore the symptoms, consult a neurologist or neurosurgeon for medical advice.
About Author –
Dr. Ravi Suman Reddy, Senior Neuro & Spine surgeon, Yashoda Hospitals – Somajiguda
MCH (NIMHANS), Advanced training in Stereotactic Radiosurgery (Brain Lab Academy – Germany). His expertise includes frameless stereotactic neurosurgery, minimal invasive spine surgery, spine stabilization, cranial micro neurosurgery, cranio-spinal trauma, and endoscopic surgery.











 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More