Knee joint preservation – Why and how its done?

At a Glance:
1. What is knee joint preservation?
2. Knee joint preservation vs. replacement, what are the indications for knee preservation?
3. What are the techniques of knee joint preservation?
4. What are the nonsurgical approaches for knee joint preservation?
5. What are the surgical procedures for knee joint preservation?
6. Postoperative rehabilitation after knee joint preservation
7. Is surgery for knee joint preservation safe, are there any risks involved?
8. How should one choose a facility for knee joint preservation surgery?
What is knee joint preservation?
Restoration of the normal motion of the knee joint and functioning without replacement is achieved by different methods of joint care and it is known as “knee joint preservation”. The approach of preserving the knee joint helps orthopedic surgeons to treat knee joint problems while retaining the natural structure of the affected joints. Techniques of knee joint preservation are used primarily in persons having defects in the articular cartilage of the knee.
Cartilage injury is a precursor to arthritic conditions and it may sometimes be manifested in the form of knee pain. The symptoms and severity of knee joint defects may vary from person to person. Traumatic injuries or age-related wear and tear often lead to damage of articular cartilage resulting in pain, stiffness and a limited range of motion. Since the articular cartilage cannot regenerate or heal by itself, intervention in the form of surgical repair is often indicated to initiate or stimulate new cartilage growth. Restoration of articular cartilage relieves a person of pain, improves normal function and can even delay or prevent the onset of arthritis in the knee joint in certain cases.
Knee joint preservation vs. replacement, what are the indications for knee preservation?
Even though joint preservation is usually a doctor’s first choice to restore the normal function of the knee joint, certain factors need to be considered while choosing between the options of knee joint preservation and knee replacement. Some of the factors that affect this decision are:
Age of the person: It is generally seen that preservation techniques tend to have more positive outcomes in younger persons, but these techniques may also be sometimes preferred in older persons who are not fit to undergo major surgery.
Weight of the person: The amount of stress placed on a joint is directly proportional to the weight of a person. A loss of even one kilogram of body weight can reduce the load on the knee joints by as much as three to five kilograms. Weight loss in case of obese individuals is one of the strategies of joint preservation.
Strength and conditioning of the body muscles: A person’s muscles not only play a vital role in the movements of the joints but also function as joint protectors by absorbing shock. Engaging in regular exercise helps in maintaining and restoring the strength of the muscles thereby reducing joint stress and pain.
Severity of the cartilage defect: The cartilage acts as a cushion between two bones of the knee joint. Thinning or erosion of smaller areas of this cartilage may be well managed with minimally invasive joint restoration procedures. However, if the cartilage loss is more, it brings the bones in direct contact with each other. The friction arising due to direct contact between the bones thereby causes their deterioration. Such cases are more suitable for joint replacement surgery.
Some of the undermentioned defects of the knee are the indications for joint preservation:
- Ligament and articular cartilage injuries due to traumatic or progressive degeneration (wear and tear).
- Meniscus tear occurs in the rubbery knee cartilage that cushions the shinbone from the thighbone.
- Osteoarthritis – inflammation in the bones and joints
- Osteochondritis dissecans – cracks in the articular cartilage and the underlying bone.
- Patellar instability occurs when the kneecap moves outside of the groove at the end of the femur bone.
- Synovial chondromatosis in the knee is a non-cancerous tumor that arises in the lining of a joint.
- Valgus or Varus malalignment, a knee deformity.
What are the techniques of knee joint preservation?
A comprehensive and customized treatment plan that takes into account a person’s age, activity level, expectations and degree of joint dysfunction is thus an important consideration in joint preservation. Multi-modality treatment options may often be a part of the comprehensive plan and include modification of physical activities, physical therapy, medications, injections and conservative surgery.
What are the nonsurgical approaches for knee joint preservation?
Physiotherapy: A lack of physical activity often leads to joint damage, physical therapy and exercise are thereby the first line of defense against such damage. It may be difficult to move during an acute episode of pain and a wrong choice of exercise can do more harm. A customized exercise regimen under the supervision of a qualified physiotherapist and orthopedic surgeon can, therefore, help in restoring the function and easing the pain.
Exercises: A tailor-made exercise schedule is beneficial in not only improving the overall health of the person but it also helps in strengthening and increasing the mobility of the muscles, ligaments and tissues around the area of the damage.
Pain Modalities like IFT, Ultrasound: Localized application of pain-relieving modalities like ice, massage, deep heat, and sometimes nerve stimulation or ultrasound is found to be helpful in certain cases.
Lifestyle modifications: Sedentary and high-stress lifestyle can be harmful to the overall health and bone health of a person. Giving up harmful lifestyle habits can help in knee joint preservation. Some of the approaches are:
Weight reduction: As stated earlier, knee joints wear the brunt of excess body weight, making them work harder. Weight management strategies under the supervision of a qualified physician can make a significant difference by taking the harmful forces away from the knee joints.
Yoga, meditation, diet modifications: Relaxation by lifestyle management techniques like yoga, meditation and diet management strategies under the supervision of a qualified dietitian can help in alleviating the pain of knee joints.
Simple Painkillers, NSAIDS: Non-steroidal anti-inflammatory drugs available over the counter help in reducing acute pain and swelling in the knee joint. Considering that long term use of such drugs can be harmful, these should be taken only under the supervision of the physician or orthopedic surgeon.
Cartilage protecting drugs: Naturally produced chemicals in the body like glucosamine and chondroitin are also available in packaged supplements over the counter. These are sometimes prescribed by doctors. While glucosamine has a role to play in the repair of joint cartilage, chondroitin acts to prevent certain other enzymes from breaking down the joint cartilage.
Off-loading braces: External aids like a knee brace or sleeve can benefit in some cases by providing relief from pressure and an increased sense of stability. Further, aids like a walker, cane, or crutches offload a person’s weight from the arthritic knee. Consequently, they can lessen the pain during walking or weight-bearing and also reduce the risk of falling.
Injections into the joint:
- Steroids: In case of a failure of NSAIDS to produce desired results, corticosteroids in the form of injections within the joint space may be prescribed to reduce inflammation. Pain relief by corticosteroids happens due to the stimulating effect of steroids on prostaglandin synthesis. Steroids also decrease the activity of collagenase and other cartilage destructive enzymes.
- Viscosupplementation with hyaluronic acid: Synovial fluid containing hyaluronic acid is a lubricant produced by the body within the joint space. Joint pain may sometimes be a symptom of a lack of hyaluronic acid. Supplementation of this acid externally in the form of injections may help ease pain and stiffness in certain cases, even though it does not stall the progression of arthritis.
- Prolotherapy (regenerative injection therapy or proliferation therapy): Injecting a natural irritant, often a form of sugar called dextrose into the soft tissue of an injured knee joint is called prolotherapy. The irritant kicks off the body’s healing response.
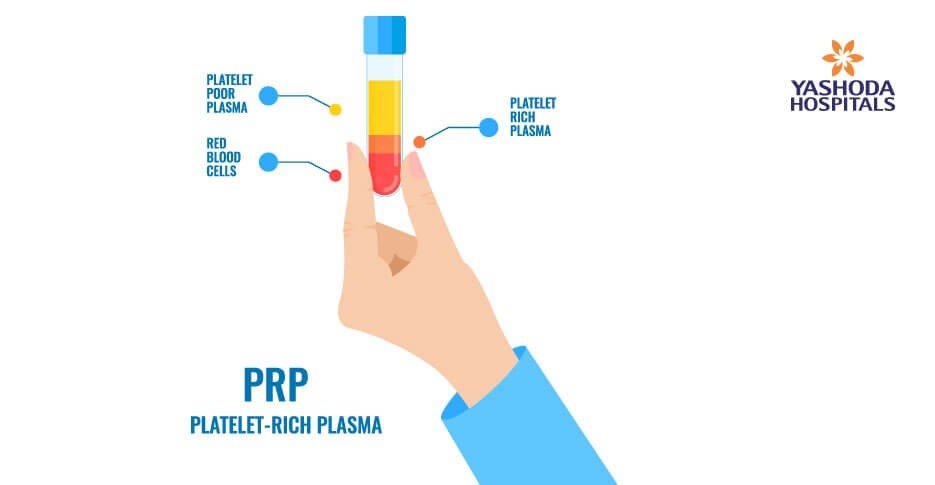
- PRP / Adipose tissue / BMAC: A concentrated form of platelets from a person’s blood is called platelet-rich plasma (PRP). Platelets not only have blood coagulation properties but they also contain proteins called growth factors that are used by the body in the process of healing injuries. PRP is sometimes used as a joint preservation approach in cases that fail to respond to more conservative options such as physical therapy, bracing and activity modification.
Radiofrequency ablation (or RFA): An electrical current from a radio wave to heat a small area of nerve tissue around the affected knee joint is delivered in this technique. Consequently, the pain signals from the affected area are lessened. RFA is generally well-tolerated and has very few associated complications.
What are the surgical procedures for knee joint preservation?
Joint preservation may also be achieved using minimally invasive surgical techniques in combination with the conservative approaches or they may be done if the conservative approaches fail. Some of the surgical approaches are:
Joint Realignment Procedures: Worn out or the arthritic parts of the knee joint can be off-loaded by surgically correcting a misaligned leg with the procedure of realignment. This helps in relieving pressure from the worn-out part of the knee thereby providing pain relief. Realignment can be done in the following ways:
- Proximal fibular osteotomy: Proximal Fibular Osteotomy is a minimally invasive day care procedure in which the fibula (calf bone) is cut and reshaped to relieve pressure on knee joint. It is a preferred alternative for pain relief from medial compartment knee osteo-arthritis. It works by transferring load to the lateral (outer) compartment and thus unloading the medial (inner) compartment of the knee. This not only reduces stress on the medial portion but also widens the joint space. Patients can stand up and walk by the afternoon of surgery, climb stairs the next day and stand for an hour or two within three or four days. A major advantage of this technique is its simplicity and ease of performance. The procedure can be done with a short incision, without damaging adjacent tissues. The procedure does not involve any internal implants. Because of all these reasons, the recovery period is shorter too.
- High tibial osteotomy: Sometimes, the knees bear the body weight asymmetrically that is typically more on the medial or inner portion of the joint (Valgus or Varus malalignment). This causes a higher amount of wear on the medial aspect than the lateral (outer) aspect of the knee joint. The leg in such a case begins to look bowed towards the inner side (bow leg). A high tibial osteotomy which is a surgical procedure for the realignment of the knee joint is indicated in certain cases like this. In this procedure, a segment of tibia (shinbone) is cut and then reshaped to relieve pressure on the knee joint. The benefits are similar to that of proximal fibular osteotomy.
- Microfracture: Tiny fractures are created in the underlying bone in the “microfracture articular cartilage repair surgical technique”. A super clot that stimulates new cartilage to develop is formed within the fracture site. The surgery is beneficial as it is quick, minimally invasive and has a short recovery time.
- Autologous chondrocyte implantation (ACI) is a surgical technique to treat isolated full-thickness articular cartilage defects of the knee. In this procedure, the orthopedic surgeon harvests a small piece of articular cartilage from the affected person’s knee. The cartilage is enzymatically treated in the lab to separate the cartilage-producing cells or chondrocytes. These cells are then grown in a culture to be implanted back in the affected area after a few weeks. The implantation is done by sewing a small patch over the articular cartilage defect and injecting the cells underneath this patch. The cells then grow and form new hyaline-like cartilage similar to the native joint cartilage.
- Arthroscopic OATS (osteoarticular transfer system): It is a surgical procedure indicated for the treatment of focal cartilage defects. Cartilage from undamaged areas of the joint is removed and surgically placed in the damaged area.
Ligament reconstruction

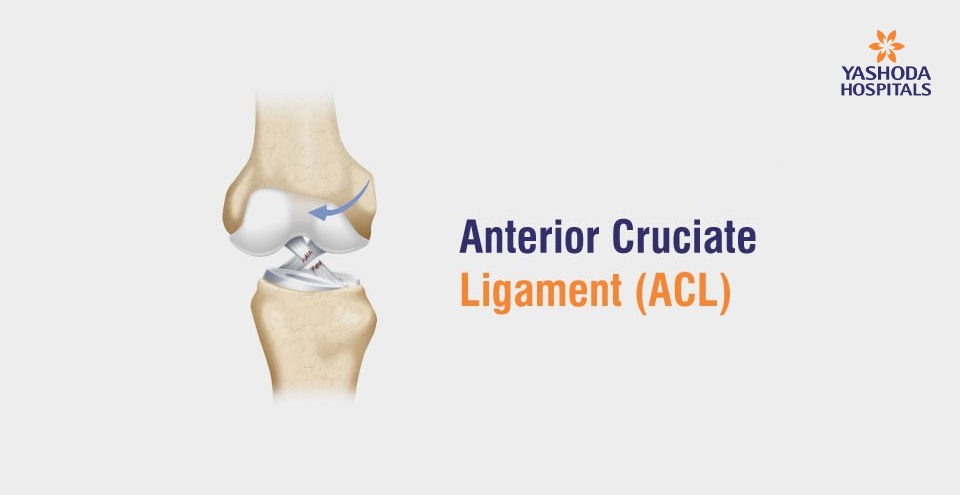
- ACL (Anterior cruciate ligament) reconstruction: This technique is performed for the repair of tears of a major stabilizing ligament of the knee, the anterior cruciate ligament. For this the surgeons make use of tissues around such as from knee cap or quadriceps. With recent advances in arthroscopic techniques, ACL surgery can now be performed as a minimally invasive procedure with low complication rates.
- PCL reconstruction: The Posterior cruciate ligament (PCL) is also a major ligament of the knee which connects the femur (bone of the thigh) to the tibia ( bone of the shin). The PCL limits the backward motion of the shinbone. Generally, surgery is considered in persons with dislocated knee and several torn ligaments including the PCL. Surgery involves reconstructing the torn ligament using a tissue graft that is taken from another part of the body.
- Meniscal repair: A meniscus is a piece of cartilage that acts as a cushion between the joint of the femur and tibia bones. This cartilage often gets damaged due to injury and wear. Repair of the torn meniscus can be done with endoscopic or keyhole surgery.
- Debridement + Lavage: Sometimes an excess of inflammatory fluid accumulation within the knee joint can cause pain. A visually guided introduction of saline solution into the knee joint by lavage or wash can help in the removal of this fluid and any loose bodies that may be present in the knee joint. Sometimes, along with lavage, the orthopedic surgeon may also do a surgical debridement or smoothening of the bone surface.
Partial Knee Replacement: In this procedure, only a part of the knee is replaced instead of the whole knee if the defect is limited only to a single area of the knee and the rest of the bone is healthy.
Postoperative rehabilitation after knee joint preservation surgery
Joint preservation surgery is very effective when it is combined with a thorough post-operative rehabilitation program and regular physical therapy to maintain the range of motion, achieve reactivation of the muscles and decrease swelling post-operatively.
Any cartilage repair procedure typically requires at least 6-8 weeks to heal and repair. Sometimes, additional aids like crutches may be required for a few weeks. A person may start on improving the range of motion and gain muscle strength after two weeks, and high-intensity physical activity like running may be undertaken after four to six months once the bone heals well.
The success of joint preservation surgery is also highly dependent upon the person working on a customized therapy plan after the surgery with a physical therapist. Maximal positive outcomes are possible only if a properly guided rehabilitation program is followed, else there may be a recurrence of stiffness, scarring, and muscle atrophy.
The actual timeframe for recovery may vary from person to person as it is dependent on a large number of factors like a person’s underlying medical health and the preservation technique used.
Is knee joint preservation surgery safe? What are the risks?
In general, the knee joint preservation surgery is a relatively low-risk and safe procedure with a low rate of complications. However, as with any surgery, there may be general and specific individual risks. Some of the commonly encountered risks are:
- Accidental damage to surrounding structures
- Infection
- Bleeding
- Pain and swelling
- Side effects of anesthesia
How should one choose a facility for knee joint preservation surgery?
Minimal invasive joint preservation surgery requires modern and innovative techniques of orthopedic surgery and sophisticated equipment. The approach towards joint preservation should be multidisciplinary including minimally invasive surgical, non-surgical and rehabilitative modalities.
The knee joint being a weight-bearing joint is subjected to lifelong pressure; as a result, it is very vulnerable to injuries and wear-tears. One of the main objectives of joint preservation is to relieve the person of pain, restore the natural functioning of the joint and avoid collateral damage to the adjacent tissues. This objective can be achieved by a precise identification of the underlying defect, sophisticated equipment used in the techniques, and surgical expertise which is usually not available in all healthcare settings. Hence the treatment is available only at a few select super-specialty hospitals in India.
The decision to have knee replacement surgery or preservation of the joint is an important one that needs to be seriously taken collectively by the affected person, family, and orthopedic surgeon. Finding the right facility and surgeon is paramount for successful outcomes and also to ensure that the person is comfortable with the decision to have surgery if needed.
Conclusion:
Joint preservation uses non-surgical or minimally invasive surgical techniques to preserve the natural functioning and structure of a deteriorating joint to delay or avoid joint replacement surgery to the maximum extent.
Being minimally invasive, joint preservation procedures offer the advantage of faster recovery and lower risk of complications and infection due to the least amount of damage to the adjacent structures.
Orthopedic surgeons specializing in joint preservation at Yashoda hospital have expertise in surgical techniques designed to preserve as much bone and function as possible. The specialists work in conjunction with physical rehabilitation experts, to constitute an experienced team to accurately diagnose and offer a full spectrum of both nonsurgical and surgical solutions.
Rehabilitation for those undergoing joint preservation should begin immediately after surgery and progress to enhance the range of motion and muscle strengthening around the joint. Rehabilitation programs should be individualized for each patient based on their medical condition and type of surgery.
References:
- PLOS One. Proximal fibular osteotomy to treat medial compartment knee osteoarthritis: Preoperational factors for short-term prognosis; Bo Liu. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197980. Accessed on October 19, 2019
- US National Library of Medicine National Institutes of Health. Joint Preservation Techniques in Orthopaedic Surgery. Available at: https://www.ncbi.nlm.nih.gov/pubmed/28632455. Accessed on October 19, 2019
- Very Well Health. The OATS Procedure. Available at: https://www.verywellhealth.com/oats-procedure-2548496. Accessed on October 19, 2019
- US National Library of Medicine National Institutes of Health. Outcomes of Joint Preservation Procedures for Cartilage Injuries in the Hip: A Systematic Review and Meta-analysis. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6009090/. Accessed on October 19,2019
About Author –
Dr. G Veda Prakash, Consultant Orthopedic & Trauma Surgeon, Yashoda Hospital, Hyderabad.
MS (Ortho), DNB (Ortho), MRCS (Ed), FRCS (Tr & Ortho)













 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More