How to Treat Severe Grade Asthma using Bronchial Thermoplasty?

According to a recently conducted nationwide survey, the burden of asthma is estimated to be around 18 million in India. The study also highlighted the growing incidence of asthma and its challenges. The complexity of the underlying clinical condition and poor response to medications in a subset of patients are reasons of concern in managing the disease.
People suffering from long-standing asthma have worsening respiratory symptoms and severe asthma attacks which may be fatal. Assessing and achieving a control on asthma manifestations will enable adults and children improve the quality of life and lead their daily activities normally.
What is Severe Asthma?
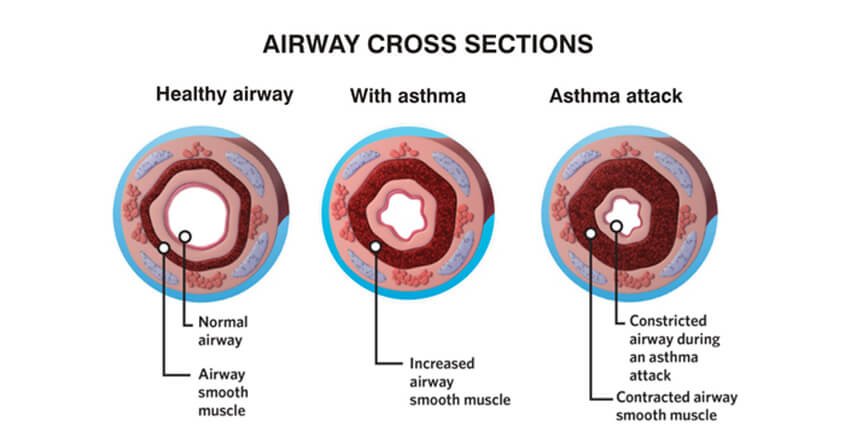
Up to 5-10 percent of the asthma patients continue to have symptoms despite optimal use of inhaled medicines. Such patients are said to have severe asthma. This is a chronic inflammatory disease of airways. Bronchial smooth muscles play a major role in maintaining the airways open for the gas exchange. In severe asthma, inflamed smooth muscles and excessive mucus take up space and make the airways lean; causing difficulty in breathing, coughing, wheezing, and tightness in chest. Patients with severe asthma have frequent asthma attacks which can either be mild or sometimes even life-threatening.
Patients with severe asthma experience troublesome symptoms that are difficult-to-control even with large doses of medications. Poorly managed symptoms worsen the quality of life which is characterized by poor sleep at night, difficulty in performing daily activities and missing school (or work).
What is an Asthma Attack?
A sudden increase in the symptoms of an asthma patient over a few hours or days is called an asthma attack. During an asthma attack, patients have a sudden increase in the blockage of airways that does not respond to rescue inhalers. This can turn out to be a life-threatening emergency. When symptoms persist despite 6-8 puffs of rescue inhaler medicines, the patients are advised to immediately call for emergency.
People who have asthma have more smooth muscle tissue surrounding their airways than people who don’t. During an asthma attack, this excess tissue constricts the airways, making it harder to breathe. Asthma medicines help open up the airways, but these medicines don’t always work well in people who have severe asthma.
What is Bronchial Thermoplasty?
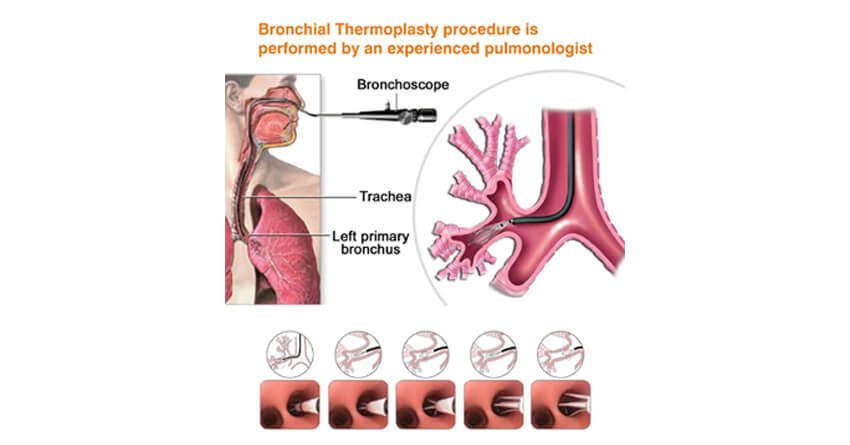
Bronchial thermoplasty (BT) is a bronchoscopic procedure which offers hope in difficult-to-treat asthma. It is a safe, minimally invasive procedure that aims to open up the narrowed airways and facilitate airflow (breathing). This is achieved by selectively reducing the thickness of the smooth muscle mass by applying radio-frequency pulses.
During the procedure, the doctor inserts a bronchoscope through mouth or nose of the patient. It is a thin, flexible tube with a small camera at the end. Once the tube is in place, he passes a special wire through the tube and then applies precisely controlled radio-frequency pulses. These pulses produce heat that is sufficient enough to reduce the thickness of the smooth muscle and opens up the airways.
Bronchial thermoplasty is performed under moderate sedation in 3 separate sessions scheduled 3 weeks apart. Each session lasts for about an hour and focuses on different regions of lungs to ensure that all the affected areas are covered. The interventional pulmonologist treats the airways of the right lower lobe, the left lower lobe and both upper lobes; in the first, second and third sessions, respectively. This step-wise approach of the procedure ensures safe and optimal outcomes.
Usually, BT is performed as an outpatient procedure and does not require any incision, this means you may be able to go home the same day.
What are the benefits and risks of bronchial thermoplasty?
So far, asthma has been treated by targeting the inflammatory response, an underlying cause of asthma attacks. Bronchial thermoplasty takes a new angle in asthma care by targeting the airway smooth muscles instead. BT enables more patent (wide and open) airway and improves respiratory symptoms and asthma exacerbations, even in patients who do not respond well to medications.
As with any procedure, bronchial thermoplasty does come with few side effects and risks. The most common side effect is a temporary worsening of respiratory symptoms. Ideally, these symptoms resolve within a week when treated with standard care. The pulmonologist will monitor the patient for possible exacerbations so as to offer prompt treatment and action plan.
What are the success rates of bronchial thermoplasty?
BT has a clinically proven 5-year success rate in patients with severe asthma. Bronchial thermoplasty is not a complete cure, the patient may still need to stay on a few inhaler medications. However, BT facilitates in reducing the dose of medication and the need of reliever inhalers.
Bronchial thermoplasty is clinically proven to –
- Decrease severe asthma attacks by 32%.
- Reduce asthma-related emergency room visits by 84%.
- Reduce days lost from work or daily activities due to asthma by 66%.
- Improve asthma-related quality of life by 79%.
Are you the right candidate for bronchial thermoplasty?
Bronchial thermoplasty is for one who:
- Has severe, persistent asthma which is difficult-to-control with inhaled corticosteroids and long-acting bronchodilator medications
- Is 18 years of age or older
- Has impaired quality of life
- Is a non-smoker
- Is not allergic to medicines required for bronchoscopy
- Does not have a pacemaker, internal defibrillator or other implantable electronic devices
If BT is not the right option for you, discuss with your pulmonologist about other treatment options to keep symptoms well managed.
A case study: This a success story of how a 53 year lady now lives a life of relief after she went through a successful bronchial thermoplasty procedure at Yashoda Hospitals.
Want to know more?
If you want to know more about bronchial thermoplasty, talk to an asthma specialist at Yashoda Hospitals. An asthma specialist or pulmonologist will guide you as to what to expect before, during and after the procedure.
References:
- Koul, P. A., & Patel, D. (2015). Indian guidelines for asthma: Adherence is the key. Lung India: official organ of Indian Chest Society, 32(Suppl 1), S1.
- Bronchial thermoplasty. Available at: https://www.asthma.org.uk/advice/severe-asthma/treating-severe-asthma/bronchial-thermoplasty/ Assessed on 23 April 2018.
- Bronchial thermoplasty. Available at: https://www.bostonscientific.com/en-US/medical-specialties/pulmonology/procedures-and-treatments/bronchial-thermoplasty.html Assessed on 15 September 2018.











 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More