Hip joint preservation – What is it and why?
At a Glance:
1. What is hip joint preservation?
2. Are you the candidate for hip preservation?
3. What are the techniques of hip joint preservation?
4. What is Core Decompression and BMAC (Bone Marrow Aspiration Concentrate)?
5. What is SUFE (Slipped Upper Femoral Epiphysis)?
6. What is containment procedures (Varus derotation osteotomy) for Perthe’s disease?
7. What is open reduction and corrective pelvic osteotomy for DDH (Developmental Dysplasia of Hip)?
8. What is arthroscopic hip joint preservation?
9. What is open hip joint preservation surgery?
10. What is postoperative rehabilitation after hip joint preservation?
11. Is hip joint preservation safe, are there any risks?
12. How should one choose a facility for hip joint preservation surgery?
What is hip joint preservation?
Hip joint preservation pertains to the preservation of a person’s native hip joint in certain cases of defects and diseases of the joint. Preservation is a multimodality approach to joint care with the following objectives:
- Restoration of the normal motion within the joint
- Functional improvement of the hip
- Elimination of pain
The common modalities of joint preservation include options like physical therapy, intraarticular injections, and surgery in isolation or in different combinations. The decision to use a particular modality depends largely on a person’s joint condition and medical needs making hip joint preservation a highly personalized approach that varies from person to person.
Are you the candidate for hip preservation?
Even though the preservation of the joint for restoring the normal function is a preferred option, positive outcomes and benefits from preservation techniques may not be realized for every person affected with a joint condition. This is so because the outcomes are highly influenced by certain factors that need to be taken into consideration while deciding on the approach to be adopted for the management of hip joint conditions. Some of the factors that affect the outcomes are considered while choosing hip preservation are:
Type of joint defect: Although hip pain is most commonly experienced by the elderly, adolescents and young adults with developmental defects of the hip known as “hip dysplasia or hip impingement” too experience pain and arthritis early in life. Hip dysplasia and femoroacetabular impingement (FAI) or hip impingement are one of the leading causes of osteoarthritis in the young and warrant a conservative surgical reconstruction or replacement of the joint. Other structural hip conditions like slipped upper femoral epiphysis (SUFE) and Perthes disease too lead to pain and arthritis as a result of adverse physical mechanics within the hip joint.
In such cases, the most desirable option is the preservation of the joint with conservative surgery in contrast to total hip replacement due to the possibility of wearing out of the artificial joint in hip replacement or the need for an early surgical revision.
Age: Preservation techniques are usually associated with improved outcomes in younger persons. However, in certain cases where an elderly person may not be eligible to undergo major surgery, joint preservation is preferred.
Weight: The hip joint is the largest weight-bearing joint of the body and it is subjected to stress throughout the life of the joint. The higher the weight of the person, the higher is the stress on the joint. Weight loss is one of the first recommendations of joint preservation in the case of obese or overweight persons.
Strength and conditioning of the body muscles: Muscles facilitate the movement of the joints and bones by contracting and relaxing. Joint movements are highly influenced by the condition and tone of the muscles and may lead to a painful condition when the muscles are not in good health. The strength of the muscles can be maintained and restored by engaging in regular exercise that helps in reducing stress on the joints and pain.
The severity of the defect of the cartilage: Joint preservation is a suitable option for treating defects of the joint cartilage when the thinning or erosion affects small areas of the cartilage. Larger defects, causing loss of a major portion of the cartilage are more suitable for treatment with total replacement surgery.
What are the techniques of hip joint preservation?
As mentioned earlier, hip preservation surgery has a threefold aim of preservation of a person’s native joint, improvement of hip function, and elimination of hip pain. Each person who may be a suitable candidate for hip preservation requires a tailored treatment plan consisting of options that include physical therapy, intraarticular injections, and surgery. A tailored treatment plan assumes greater importance here because not all hip pain is the same. In certain conditions, one modality that may be helpful for a person may cause further damage to the joint of another.
Hip preservation surgery also aims at preventing or delaying arthritis and retain the health and activity levels of affected adolescents and young adults. Correction of defective hip mechanics can help in easing pain and improving the longevity of the joint.
Surgical interventions for hip joint preservation constitute the lesser invasive hip arthroscopy procedure or open hip surgery. In certain cases, there may be a need for realignment or reshaping of the pelvis or femur and in certain cases, hip reconstruction may be indicated instead of hip preservation. Depending on the individual needs of the person and the joint anatomy the doctors try to choose the most feasible option from amongst the various new minimally invasive hip reconstruction and replacement techniques, some of which are as mentioned here:
- Core Decompression and BMAC(bone marrow aspiration concentrate) for AVN (Avascular Necrosis) / Osteonecrosis
- In-situ fixation / open reduction and internal fixation for SUFE (Slipped Upper femoral epiphysis)
- Containment procedures (Varus derotation osteotomy) for Perthes disease
- Open reduction and corrective pelvic osteotomy / Femoral osteotomy for DDH (Developmental Dysplasia of Hip)
- Arthroscopic procedures:
- Labral repair
- FAI (femoro-acetabular impingement)
- Debridement for CAM, Pincer lesions
- Open surgery:
- Surgical dislocation
- GANZ trochanteric flip, Z-capsular cut hip joint dislocation
- Head reduction in COXA MAGNA
- Excision or removal of the synovium in PVNS (Pigmented Villonodular synovitis)
- Removal of multiple loose bodies in synovial chondromatosis
- Cartilage and bone grafts
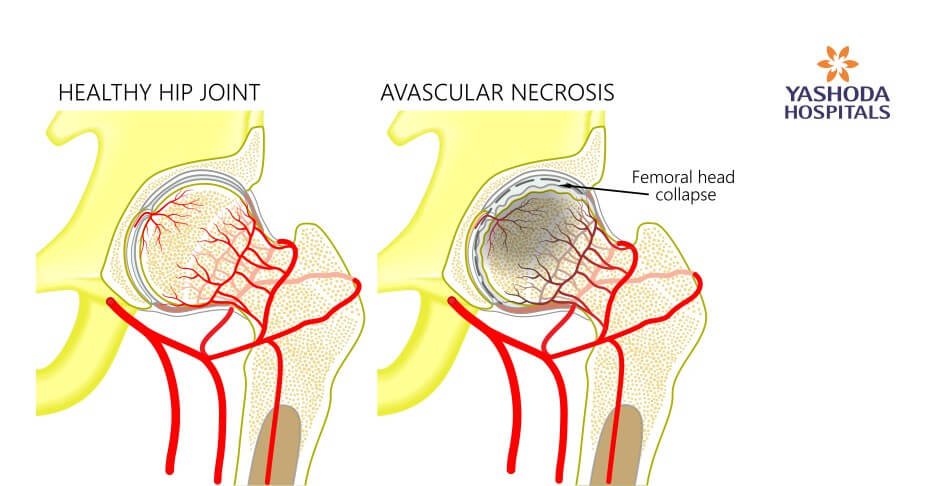
What is core decompression and BMAC (bone marrow aspiration concentrate) for AVN (Avascular Necrosis) / Osteonecrosis?
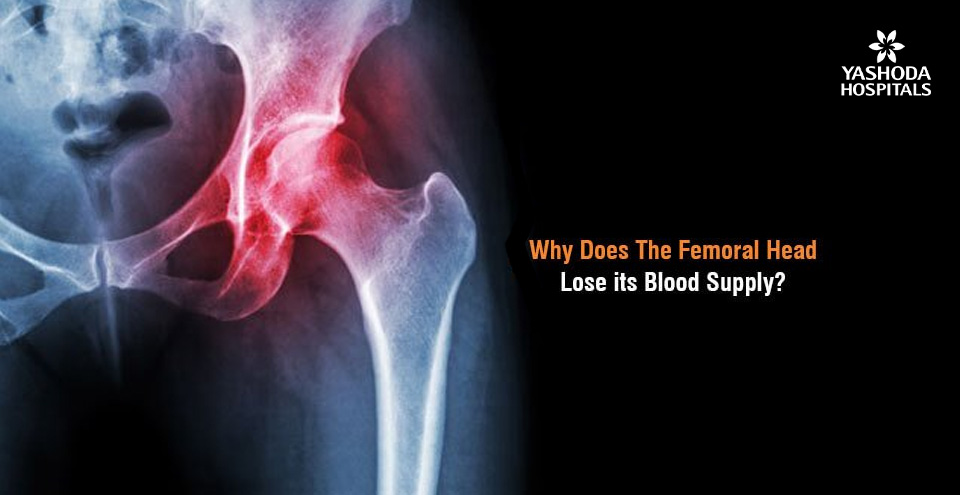
A decreased blood flow to the head of the femoral bone due to trauma or certain medical conditions can cause necrosis and microfractures within the bone and collapse of the articular surface of the bone in later stages. Core decompression is a popular and effective technique for the treatment of early AVN of the femoral head. The procedure involves surgical drilling into the area of the dead bone of the joint. As a result, the pressure is decreased which facilitates increased blood flow and delay or even stops in certain cases, the destruction of the joint or the bone. Sometimes, in addition to core decompression, an additional procedure called the bone marrow aspirate concentrate (BMAC) is performed. BMAC is a regenerative therapy procedure that makes use of the person’s bone marrow cells to initiate healing.
What is in-situ fixation / open reduction and internal fixation for SUFE (Slipped Upper Femoral Epiphysis)
A Slipped Upper Femoral Epiphysis (SUFE) is a condition that affects the epiphyseal plate or the growth plate of the hip joint in children. The epiphyseal plate is an area of growing tissue where the lengthening of the bone takes place. In SUFE, the growth plate suffers a kind of fracture leading to the slipping out of the head of the femur from its position. The treatment of choice is surgical, but the type of operation depends on the extent to which the head of the femur has slipped. Surgery is done to stabilize the growth plate and to stop it from slipping more. A surgical screw is inserted across the growth plate and secured to the head of the femur. A few days of bed rest after the surgery is advised, followed by the use of crutches while walking to keep the weight off the hip joint.
What are the containment procedures (Varus derotation osteotomy) for Perthes disease?
Legg-Calve-Perthes disease affects children. The blood supply to the femoral head or the ball part of the hip joint gets interrupted temporarily in this condition due to which the bone begins to die. The femoral may weaken and fragment as the condition progresses. Sometimes, the bone may even break apart thereby losing its round shape. The goal of treatment of Perthes disease is threefold, relief of painful symptoms, protection of the femoral head’s shape and restoration of the normal movements of the hip.
The femoral head can get deformed if left untreated and may stop fitting within the socket of the acetabulum of the hip bone. This can cause further problems like the early onset of arthritis. Osteotomy is the most commonly preferred surgical intervention for the treatment of Perthes disease. In an osteotomy, the femoral head is repositioned to be placed snugly within its socket. The alignment is maintained by placing screws and plates within the bone. Sometimes, the femur bone maybe cut surgically to realign the joint or the socket may be made deeper to fit the enlarged head of the femur.
What is open reduction and corrective pelvic osteotomy / Femoral osteotomy for DDH (Developmental Dysplasia of Hip)?
Chronic hip pain is a common sign of conditions of the hip that are associated with aging. When chronic pain is reported in adolescents and young adults, hip dysplasia is often suspected to be the underlying cause. Hip dysplasia is a condition where one or more areas of the hip joint develop abnormally. Preservation of the hip for as long as possible is the main consideration in the treatment of persons with hip dysplasia. Hence hip pain in adolescents and young adults should be evaluated promptly. Corrective pelvic osteotomy consists of a series of cuts within the bone for reorienting the acetabulum over the head of the femur. The normal anatomy is thereby restored. This position is then stabilized by placing screws in the bones.
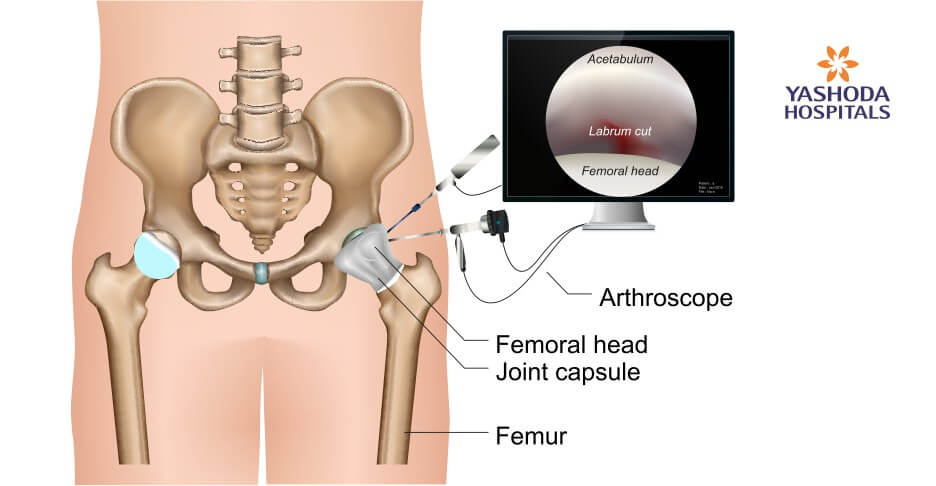
What are arthroscopic hip preservation procedures?
Arthroscopy is a minimally invasive surgical technique that allows the orthopedic surgeon to visualize and do the surgical procedure through small incisions and instruments. Some of the arthroscopic procedures for hip preservation are:
Arthroscopic labral repair: The labrum is a ring of cartilage surrounding the hip socket. It cushions the hip joint and functions as a rubber seal to hold the femoral head securely within the socket of the hip. This cartilage may get torn during trauma or structural abnormalities. The treatment of choice for labral repair is arthroscopic surgery.
Arthroscopic procedure for FAI (femoro-acetabular impingement): An overgrowth of the bone called bone spurs that develop around the femoral head or acetabulum leads to abnormal contact between the hip bones. As a result, the movement of these bones gets hampered. Osteoarthritis may develop due to a long-standing FAI. In such cases, when surgery is indicated, it can be usually done with hip arthroscopy for removing the abnormal bone and stabilizing the cartilage.
Arthroscopic debridement for CAM, Pincer lesions: An abnormally shaped femoral head known as CAM impingement or a hip socket that overcovers the femoral head known as Pincer impingement, may cause interference in the smooth movements of the femoral head within the hip socket. As a result, labral cartilage gets damaged. Arthroscopic debridement for removal and flushing away of loose bodies are recommended to correct impingement deformities of the hip.
What is open surgery for hip preservation?
As the name implies, open surgery is done through a large, open-cut or incision in the skin. Considering some of the limitations of minimally invasive surgery, a larger incision is required to gain more extensive visualization and access to the hip joint. Some procedures for hip preservation are thus performed using the open surgery approach. A few examples are:
Safe surgical dislocation: For certain fractures of the hip a procedure called safe surgical hip dislocation (SHD) that allows full access to the femoral head and acetabulum is performed. The advantage of SHD is that it avoids the risk of femoral head avascular necrosis or post-traumatic arthritis. Associated acetabular or labral lesions can also be repaired simultaneously using this approach.
GANZ trochanteric flip, Z-capsular cut hip joint dislocation: A Ganz trochanteric flip is a surgical technique for hip dislocation that provides access to the femoral head and acetabulum within the hip joint without posing a risk of avascular necrosis of the head. The Z-capsular cut technique protects the main blood vessels from getting damaged during the surgery.
Head reduction in COXA MAGNA: Coxa Magna is a condition in which there is a circumferential, asymmetrical enlargement and deformation of the head of the femur and its neck. Intra-articular osteotomy surgery is performed for head reduction by making it more spherical.
Excision or removal of the synovium in PVNS (Pigmented Villonodular synovitis): PVNS is a condition where the lining of the joints and tendons known as the synovium becomes thickened and overgrown. Excess fluid is secreted by this synovium thereby causing swelling in the joint and painful movements. In the case of diffuse PVNS that affects the whole of the hip, the entire joint lining may need to be removed which is preferably done by open surgical technique.
Removal of multiple loose bodies in synovial chondromatosis: In synovial chondromatosis, nodules made of cartilage develop due to abnormal growth of the synovium. Sometimes, these nodules may just break off and lay loose inside the joint thereby causing pain and related joint problems. Open surgery is usually recommended as a treatment for synovial chondromatosis to remove the loose bodies along with partial or complete synovectomy.
Cartilage and bone grafts: Cartilage and bone grafting is a surgical procedure in which a natural bone or an artificial replacement material is placed into the space between or around the affected bone or cartilage to promote healing.
What is postoperative rehabilitation after hip joint preservation?
Joint preservation surgery can realize positive outcomes to the maximum extent only when a personalized postoperative rehabilitation program is planned and adhered to after the surgery. Regular physical therapy for at least 1-2 weeks or as advised by the physical therapy expert and the orthopedic surgeon is crucial in maintaining the range of motion, achieve reactivation of the muscles and decrease post-operative swelling.
It usually takes 6-8 weeks for the tissues to heal after a cartilage repair procedure. The use of supportive aids like braces or crutches for a few weeks may sometimes be advised by the doctor. Improvement in the range of motion and gain in muscle strength may become evident in about two weeks but it usually takes four to six months for the bone to heal well.
The success of joint preservation surgery is highly dependent upon the person’s lifestyle and medical condition. Positive outcomes are possible only if a properly guided rehabilitation program is followed else there may be a recurrence of stiffness, scarring, and muscle atrophy. Consequently, the time of recovery may vary from person to person as it is largely dependent on the factors mentioned above.
Is hip joint preservation surgery safe? What are the risks?
In general, hip joint preservation surgery is a safe procedure with a relatively low rate of complications in comparison to other major surgeries. However, even the smallest surgery is not devoid of certain inherent risks. There may be general and specific individual risks associated with hip preservation surgery too. Some of the commonly encountered risks are:
Side effects of anesthesia that may include but is not limited to:
- Drowsiness
- Headache
- Heart attack or stroke in extremely rare cases
- Nausea
- Sore throat, due to the breathing tube if used during surgery
Risks associated with the procedure:
- Accidental damage to surrounding structures, including vessels, nerves, or adjacent cartilage.
- Infection at the site of surgery
- Bleeding
- Pain and swelling
How should one choose a facility for hip joint preservation surgery?
Joint preservation is a multi-modality approach that includes person-specific use of open or minimally invasive surgeries, non-surgical techniques, and rehabilitation. Medical care for hip preservation which is a relatively new field should be considered at an institution where these multidisciplinary treatment options including surgical and rehabilitation expertise and infrastructure are available. Such kind of treatment facility is available only at a few select super-specialty hospitals in India.
Conclusion:
The total joint replacement technology has limitations like the need for revision surgery and wearing of the implant thereby affecting lifestyle activities in younger age groups. Thus, preservation of the natural joints for as long as possible is desirable. Being minimally invasive, certain joint preservation procedures have the advantage of faster recovery and lower risk of complications and infection due to the least amount of damage to the adjacent structures.
Rehabilitation for persons undergoing joint preservation should begin immediately after surgery and progress to enhance the range of motion and muscle strengthening around the joint. Rehabilitation programs should be customized to the needs of each person based on their medical condition and type of surgery.
Joint preservation is an emerging field in orthopedics but is available only at select centres in India. Orthopedic surgeons specializing in joint preservation at Yashoda hospital have expertise in surgical techniques designed to preserve as much bone and function as possible. The specialists work in conjunction with physical rehabilitation experts, to constitute an experienced team to accurately diagnose and offer a full spectrum of both nonsurgical and surgical solutions. At Yashoda hospital hip joint preservation techniques focus on resolving conditions like femoroacetabular impingement, repair of labral and chondral tears resulting from hip impingement, carrying out cartilage repair and regeneration and treating complex conditions like tendinopathies to name a few.
References:
- Core Decompression Augmented With Autologous Bone Marrow Aspiration Concentrate for Early Avascular Necrosis of the Femoral Head Lucas Arbeloa-Gutierrez, M.D., Chase S. Dean, M.D., Jorge Chahla, M.D., and Cecilia Pascual-Garrido, M.D. Available at. https://www.drpascualmd.com/pdf/core-decompression-with-bmac.pdf.Accessed on November 10, 2019
- Open reduction of slipped capital femoral epiphysis. Available at: https://www.nice.org.uk/guidance/ipg511/chapter/1-Recommendations. Accessed on November 10, 2019
- https://orthoinfo.aaos.org/en/diseases–conditions/femoroacetabular-impingement/
- Journal of Orthopaedic Surgery. Surgical dislocation of the hip without trochanteric osteotomy, Daniel Schweitzer, Ianiv Klaber. Available at: https://journals.sagepub.com/doi/full/10.1177/2309499016684414. Accessed on November 10, 2019
- American Academy of Orthopedic Surgeons. Synovial Chondromatosis. Available at. https://orthoinfo.aaos.org/en/diseases–conditions/synovial-chondromatosis. Accessed on November 10, 2019
About Author –
Dr. Praveen Mereddy, Consultant joint Replacement & Trauma Surgeon, Yashoda Hospitals – Hyderabad
MS (Ortho), DNB (Ortho), MRCS (Ed), M.Ch (Ortho), FRCS (Ortho)
Complex Primary Hip and Knee Replacement Surgery, Partial Knee Replacement Surgery, Treatment of Painful/Unstable/Failed (Loosening/infection) Primary Joint Replacements, Complex, complicated fractures and Pelvi-acetabular trauma














 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More