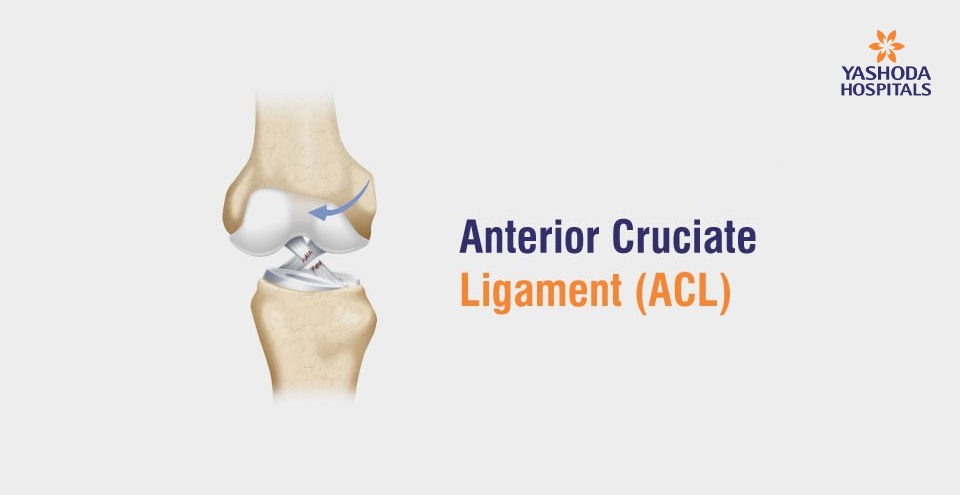
Anterior Cruciate Ligament
by Dr. Shashi Kanth G | Jan 08, 2021 | Bones & Joints | 5316 73
<< Previous Article
Spyglass CholangioscopyNext Article >>
Comprehensive Approach for Obesity చుండ్రు సమస్య : ఎందుకు వస్తుంది? మరియు సమర్థవంతమైన పరిష్కారాలు
చుండ్రు సమస్య : ఎందుకు వస్తుంది? మరియు సమర్థవంతమైన పరిష్కారాలు రోసేసియా : కారణాలు, లక్షణాలు, చికిత్స, నివారణ
రోసేసియా : కారణాలు, లక్షణాలు, చికిత్స, నివారణ మెడనొప్పి : కారణాలు, లక్షణాలు, చికిత్స, నివారణ
మెడనొప్పి : కారణాలు, లక్షణాలు, చికిత్స, నివారణ Good Yeast Gone Bad! Yeast Infection Causes, Symptoms, and Treatment
Good Yeast Gone Bad! Yeast Infection Causes, Symptoms, and Treatment Overcoming Stigma! The Modern Way To Treat an Age-Old Epidemic Called Syphilis
Overcoming Stigma! The Modern Way To Treat an Age-Old Epidemic Called Syphilis