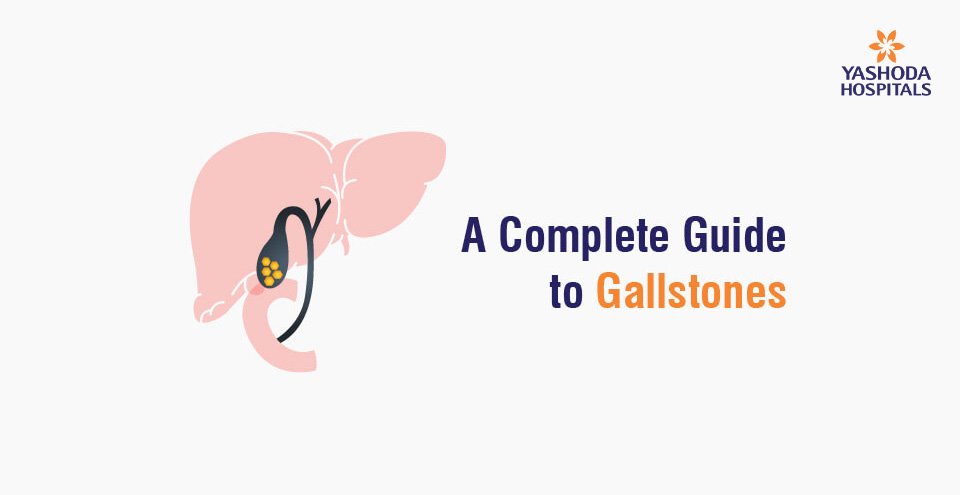
A Complete Guide to Gallstones
Gallstones, also known as cholelithiasis, are a common and potentially painful condition that affects millions of people worldwide. This guide provides a comprehensive overview of gallstones, including their causes, symptoms, diagnosis, and treatment options. We will also discuss how to prevent gallstones and what lifestyle changes you can make to reduce your risk. By the end of this blog, you will have a better understanding of gallstones and how to manage them.
How are gallstones formed?
The gallbladder is a small organ located on the upper right side of the abdomen, just below the liver. It stores and concentrates bile, the digestive fluid produced by the liver.
Gallstones form when bile hardens into solid particles due to an imbalance in the chemical make-up of bile in the gallbladder, resulting in an excess accumulation of cholesterol, bilirubin, or calcium in the bile. The gallstones grow in the gallbladder and can be as big as golf balls or as small as sand grains.
Additionally, infections in the biliary system, which may also act as an initiating factor in stone formation, may cause damage to the mucosal lining of the gallbladder, leading to the development of gallstones.
Gall bladder stones are characterised by right upper abdominal pain, fever, vomiting, or jaundice
What are the signs and symptoms of gallstones?
The most common signs and symptoms of gallstones include
- Abdominal pain (upper right abdomen below the ribs or the centre of your stomach that is dull, aching, and continuous)
- Nausea and vomiting
- Fever
- Chills
- Jaundice
- Clay-coloured stools
- Indigestion
- Bloating and Gas
- Uncontrolled blood sugar levels (in diabetics)
Sometimes, gallstones can be asymptomatic (especially in individuals with chronic diabetes) and not cause any symptoms. Typically, they are discovered during a routine medical exam or imaging test. They are usually small and do not require treatment. However, if they grow in size, they can cause pain and other symptoms and may require medical intervention.
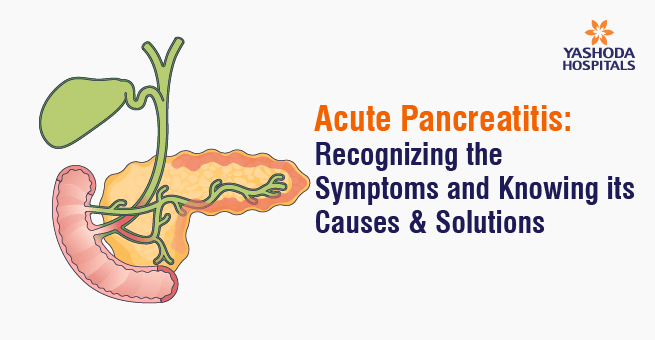
What are the complications of gallstones?
The most common complication of gallstones is cholecystitis (inflammation of the gallbladder), resulting in severe abdominal pain, nausea, vomiting, and fever.
Other complications include blockage of the common bile duct, which can lead to jaundice, cholangitis (infection of the bile ducts), and pancreatitis (inflammation of the pancreas). In rare cases, gallstones can cause gallbladder perforation (a tear in the gallbladder wall), which can be life-threatening.
What are the risk factors for gallstones?

Gallstones impact a variety of people. The following are possible risk factors for gallstones:
- Gallstones are twice as likely to develop in women than in men.
- Gallstones are more common in people over 60 years of age than in younger people.
- Obesity, particularly in women, is a significant risk factor for gallstones.
- Rapid weight loss causes the liver to release additional cholesterol into the bile, which can result in gallstones.
- Fasting reduces gallbladder movement, which results in an excess of cholesterol in the bile.
- Diabetes is associated with elevated levels of fatty acids known as triglycerides, which increase the risk of gallstones.
- Excess oestrogen during pregnancy, hormone replacement therapy, or birth control pills appear to raise cholesterol levels in bile while decreasing gallbladder movement, both of which can result in gallstones.
- Drugs that lower cholesterol in the blood increase the amount of cholesterol secreted in bile, thereby increasing the risk of gallstones.
- Additionally, having a family history of gallstones is often associated with a higher risk.
How are gallstones diagnosed?

Tests and procedures used to diagnose gallstones and their complications include the following:
Blood tests: Blood tests help to reveal the signs of infection or inflammation of the bile ducts, gallbladder, pancreas, or liver, or other complications caused by gallstones.
Imaging tests: Imaging tests such as abdominal ultrasound, endoscopic ultrasound, cholecystography, magnetic resonance cholangiopancreatography (MRCP), or endoscopic retrograde cholangiopancreatography (ERCP), among others, help to confirm the presence of gallstones.
- Abdominal ultrasound is the most commonly used imaging test for gallstones. It uses sound waves to create images of the gallbladder.
- Endoscopic ultrasound combines the use of an endoscope, a small, flexible tube inserted into the digestive tract, with an ultrasound machine, which produces images using sound waves. It can be used to detect smaller stones that may not be visible on an abdominal ultrasound.
In unconfirmed cases, endoscopic ultrasound, the gold standard for lower common bile duct (CBD) stones, may help in identifying stones in the lower part of the bile duct, which is then followed by ERCP for removal. - Additional tests may include an oral cholecystography, a hepatobiliary iminodiacetic acid (HIDA) scan, a CT scan, a MRCP, or an ERCP. When stones have slipped down the gall bladder into the bile duct or the common channel, they are best diagnosed with MRCP or ERCP.
What are the treatment options for gallstones?
Treatment options for gallstones are determined by the size and type of stones as well as the symptoms they cause. Small gallstones that do not cause symptoms may not necessitate treatment. In this case, the doctor may advise regular checkups to monitor the gallstones.
However, if the gallstones are causing symptoms, your doctor may advise one of the following treatments:
- Medication: Medication can be used to dissolve gallstones. This is typically done with bile acid medications, which aid in the breakdown of gallstones. This treatment is only useful for small gallstones, and it can take months to work.
- Surgery: The most common treatment for gallstones is surgery. A cholecystectomy is the most common type of surgery, and it involves the removal of the gallbladder. This is usually done laparoscopically, which is a minimally invasive procedure.
Patients may need to have an ERCP with stone removal before having their gallbladder laparoscopically removed, typically 24 hours apart, if they have complicated gallbladder stones (jaundice, cholangitis, and pancreatitis).
Patients who had a laparoscopic gallbladder removal with no surgical complications should be able to walk after 4 hours, start a liquid diet after 6 hours, and resume their regular diet after 12 hours.
- Shock Wave Lithotripsy: This procedure uses shock waves to break up the gallstones and is usually done in cases where the gallstones are too large to be dissolved with medication.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure involves removing gallstones by inserting a tube into the gallbladder. This is usually done in cases where the gallstones are too large to be dissolved with medication or broken up with shock waves.
What are the preventive measures?
Preventive measures for gallstones include:
- Eating a healthy diet: A balanced diet low in fat and cholesterol can help lower the risk of developing gallstones. It is important to consume a variety of fruits and vegetables, whole grains, and lean proteins that can help you maintain a healthy weight and lower your risk of gallstones.
- Keeping a healthy weight: Being overweight or obese increases your chances of developing gallstones. Losing weight gradually and maintaining a healthy weight can help reduce the risk of gallstones.
- Staying active: Regular physical activity can help you maintain a healthy weight and lower your chances of developing gallstones.
- Avoiding crash diets: Crash diets can result in rapid weight loss, which increases the risk of gallstones.
- Limiting alcohol consumption: Drinking too much alcohol can increase the risk of gallstones.
- Taking medications: Certain medications, such as birth control pills and cholesterol-lowering drugs, can increase the risk of gallstones. Talk to your doctor about any medications you are taking and their potential risks.
- Taking supplements: Taking supplements such as vitamin C can help reduce the risk of gallstones. However, unregulated use of vitamin C can increase your chances of developing kidney stones; therefore, it is always recommended to take supplements only as prescribed by a doctor.
What is the outlook for people with gallstones?
The majority of people with gallstones have no symptoms and do not require treatment. However, if symptoms do occur, treatment options such as medications, dietary changes, and surgery may be recommended. With proper treatment, the majority of people with gallstones can expect to have a good outcome.











 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More