Percutaneous Coronary Intervention of A Diffusely Degenerated Saphenous Vein Graft: A Road Less Taken
Background
63-year-old-female presented with complaints of shortness of breath on exertion since 1 week and bilateral pedal oedema since 3 days. Six years ago, she had undergone CABG with SVG to LAD and LCX. Also, she had undergone PCI to mid segment of LAD using bare metal stent before 10 years. She was a known case of hypertension and bronchial asthma.
Diagnosis
Upon examination at admission, pulse rate was 80 per minute and blood pressure was 120/80 mm Hg. Biochemical and Haematological reports were normal. Electrocardiograph showed ST-segment of V1-4 suggestive of ischemia of anterior wall. Echocardiography demonstrated mild left ventricular dysfunction with regional motion abnormalities of anterior wall, apex and moderate mitral regurgitation. Angiography of native coronary arteries revealed distal LMCA, critical stenosis with mid segment in-stent occlusion of the LAD with bridging collaterals. The LCX was non-dominant, with proximal mild disease, followed by total occlusion. The RCA was dominant artery with 50% stenosis of the distal segment. The graft angiography revealed tinned out streaky degenerated SVG to LAD with anastomotic stenosis and SVG to LCX was patent.
Treatment
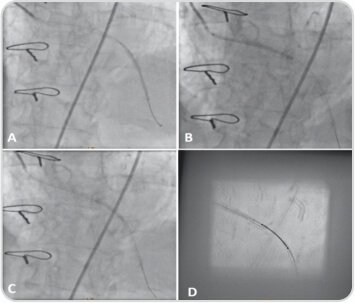
The patient was advised to undergo PCI for treating the SVG lesion as intervention of the native LAD was thought to be more complex. After injection of 100 units/kg of unfractionated heparin, the SVG graft was cannulated with a 6Fr. AL-2 guide catheter through right femoral approach. At the very first attempt, the SVG-LAD graft lesion was successfully crossed with a 0.014″ Gaia-2 guide wire and caravel microcatheter support & wire tip was placed in distal LAD (Figure 1B). The LAD lesion was pre-dilated with 1.2×8 mm and 2.0×12 mm balloons at 12 atm for 15″sec. The 0.014″ Gaia-2 guide wire was exchanged with Versa Turn guide wire (Figure 1B). The Distal SVG-LAD graft lesion was stented with 2.25×44 mm sirolimus-eluting stent (SES), deployed at 12 atm for 20″sec. Subsequently, proximal SVG-LAD graft lesion was stented with 2.5×48 mm Supralimus Grace SES deployed at 12atm for 20″sec. Another overlapping stent was placed in mid SVG-LAD graft lesion and stented with 2.5×20 mm Supralimus Grace SES deployed at 12 atm for 20″sec (Figure 2). Post-dilation was done with 2.5x 15 mm non-compliant balloons up to 14-18 atms. Post procedure angiogram showed no residual stenosis/dissection with TIMI III flow in= SVG-LAD graft. (Figure 3)
After the procedure, two-dimensional echocardiography showed trivial tricuspid valve regurgitation (RVSP: 27 mmHg), mild mitral valve regurgitation (jet area: 5.0 sqcm) and mild aortic valve regurgitation (PPG /MPG:24/17 mmHg), mildly dilated left atrium, left ventricular regional wall motion abnormality was present (mid, distal, apex hypokinetic). However, left ventricular systolic function was normal (EF – 60%), with grade-I LV diastolic dysfunction.
There was no pericardial effusion/vegetation/clot. She was stabilised in ICCU, post-procedure. She was discharged in hemodynamically stable condition. She is in favourable condition, without any related complaints up to 4 months follow-up after the PCI procedure.
Discussion
SVGs are more vulnerable to occlusion or degeneration, as compared to native coronary arteries, such that within 10 years after coronary artery bypass graft (CABG) surgery, about only 60% of SVGs remain patent(1). In addition to occlusion, SVGs are more prone to degeneration, increased neointimal hyperplasia and aggressive atherosclerosis; and have been associated with plaque embolization and the no-reflow phenomenon. All these characteristics lead to challenging interventional procedures in SVG.
With increasing numbers of CABG surgeries being performed worldwide, restenosis rates in SVGs has also been amplified, especially after more than 5 years post-CABG. This has in turn resulted into increased graft interventions. However, PCI in SVGs is rather more difficult than the native coronaries. Due to difference in morphology and physiology of SVGs, proper selection of stents, embolic protection devices, with application of good procedural techniques are required such that complications could be diminished.
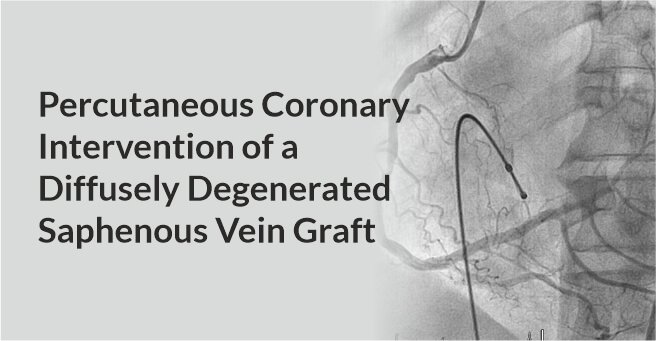
Coronary angiogram images showing that
(A) Gaia-2 wire tip was placed in distal LAD with support of Caravel microcatheter
(B) Lesion was pre dilated with 1.2 x 8 mm, 2.0×12 mm at 12 atm for 15 sec then Gaia-2 wire was exchanged with VersaTurn guide wire
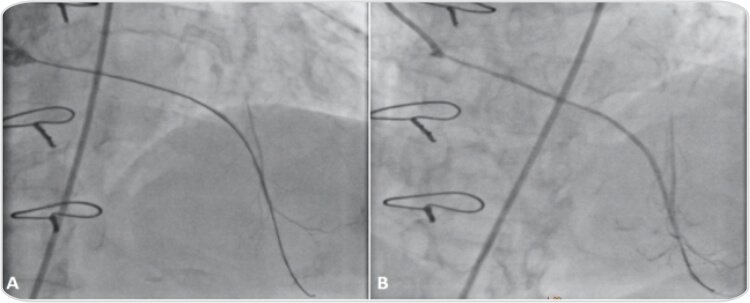
Coronary angiogram indicating
(A) The distal SVG-LAD graft deployed with 2.25 x 44 mm Supralimus Grace at 12 atm for 20 sec
(B) The proximal SVG-LAD graft deployed with 2.5 x 48 mm Supralimus Grace at 12 atm for 20 sec
(C) The mid SVG-LAD graft deployed with 2.5 x 20 mm Supralimus Grace at 12 atm for 20 sec, by overlapping proximal and distal stents
(D) Stent booster Image of Supralimus Grace (2.5 x 20 mm) in the mid SVG-LAD graft, overlapping proximal and distal stents.
Post PCI angiogram showing good TIMI flow in SVG-LAD graft
About Author –
Dr. Pankaj Vinod Jariwala, Consultant Interventional Cardiologist, Yashoda Hospitals – Hyderabad
MD, DNB, DNB, MNAMS, FICPS, FACC.
Fellowship in Interventional Cardiology [ICPS, Paris, France]He has performed 5000+ percutaneous trans-luminal coronary Angioplasty & 10,000+ Coronary Angiograms and treated 500+ structural heart diseases (including congenital) with Percutaneous Balloon Mitral Valvuloplasty [PBMV] and other pediatric & adult cardiac interventions.







 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

