How to treat and prevent Peripheral vascular disease?
At a Glance:
1. What is peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
2. What are the types of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
3. What are the causes of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
5. What are the symptoms of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
6. How is peripheral artery disease (PAD) or peripheral vascular disease (PVD) diagnosed?
7. What are the stages of peripheral vascular disease?
9. What is the treatment of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
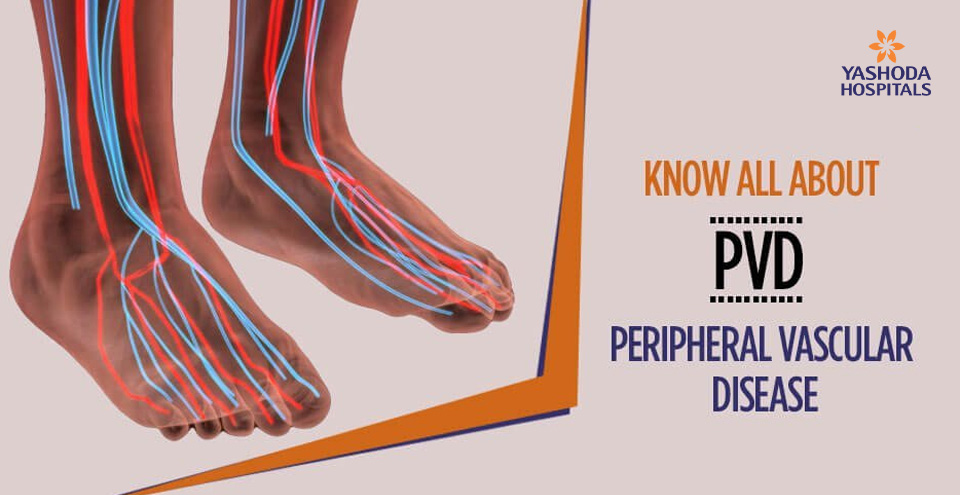
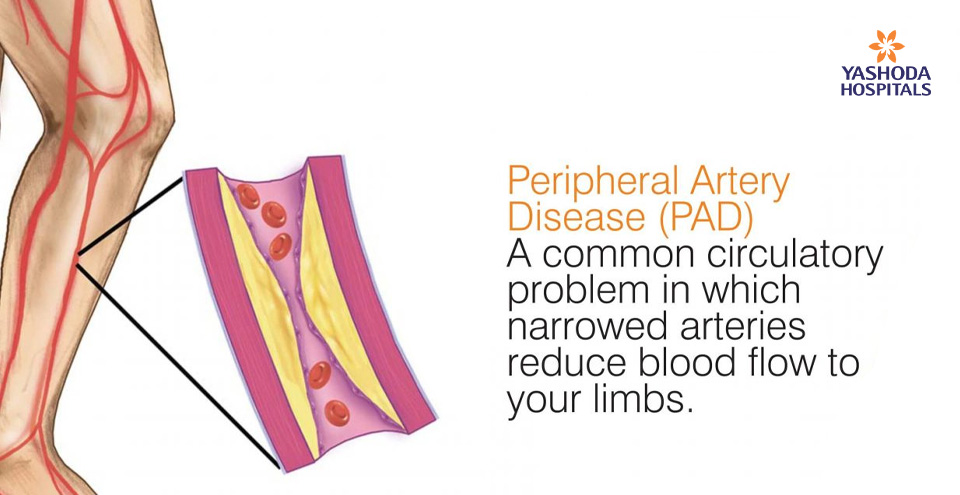
What is peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
Peripheral vascular disease (PVD), also termed as peripheral artery disease is a disorder of blood circulation, seen commonly in the lower limbs. Pathological narrowing down of arteries reduces the blood flow to limbs resulting in the symptoms of the disease.
Peripheral artery disease may also be a sign of accumulation of fatty deposits i.e. atherosclerosis in the arteries all over the body.
In India, peripheral vascular disease is an important cause of morbidity which is often overlooked due to lack of awareness amongst the general population. It is estimated that more than 10 million people in India could be affected by the disease. Amongst the patients affected, an estimated 40% of patients having coronary artery disease also have associated peripheral artery disease. It is further estimated that nearly 14% of these patients may have carotid artery stenosis and 17% have renal artery stenosis. Studies also suggest that the prevalence of the peripheral vascular disease in diabetics in India could be as high as 36%.
What are the types of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
Peripheral vascular disease may be of different types depending on the site affected and the underlying pathology. Some of the commonly reported types are:
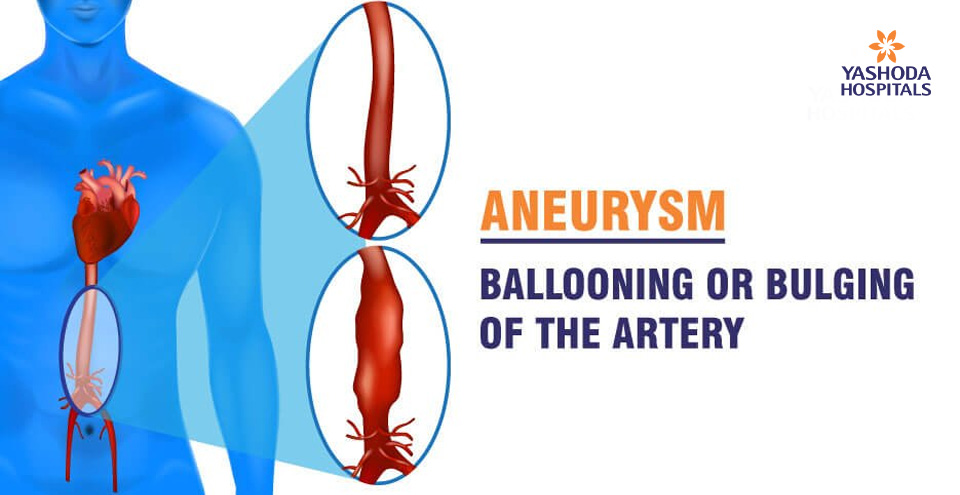
- Peripheral artery disease: Build-up of atheromatous plaques within the arteries supplying blood to the arms and legs. The arteries become narrow due to the build-up of plaque, leading to their blockage.
- Buerger’s disease: Inflammation of the small blood vessels causes them to swell up and become narrow. These vessels may often get blocked by clots of blood. The arms and legs are the most affected regions.
- Erythromelalgia: This type of peripheral vascular disease is manifested by symptoms like a burning pain, increased body temperature, erythema and swelling of the skin. The hands and feet are mainly affected.
- Raynaud’s disease: A rare peripheral vascular disease where spasm of blood vessels cause reduced blood flow when exposed to cold. Typically the fingers of the hands are affected.
- Renal artery stenosis: Narrowing of artery that supplies blood to the kidneys from the heart, mostly due to atherosclerosis or fibromuscular dysplasia.
What are the causes of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
The most common underlying cause of PVD is ‘atherosclerosis’ where fatty deposits known as plaques accumulate in the walls of the artery walls and reduce blood flow due to constriction.
There is a myth that atherosclerosis is usually present in the blood vessels of the heart. The fact is that the disease affects the arteries throughout the body including the arteries of the limbs thereby causing peripheral vascular disease.
Other less common causes of PAD may include:
- Aberrant or unusual anatomy of the ligaments or muscles
-
Excessive exposure to radiation
- Inflammation of the blood vessels
-
Injury to the limbs

What are the risk factors for peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
Factors that increase the risk of atherosclerosis also increase the risk of PAD. Some of the general factors to be considered are age, sex, and ethnicity. PVD is observed to be twice as common in males as compared to females.
Some of the individual factors that increase a person’s risk of suffering from PVD include (in alphabetical order):
- Age: Individuals over age 50 years
- Dyslipidaemia high blood cholesterol: An abnormally high level of cholesterol or fat in the blood is strongly associated with PVD.
- Family history of high cholesterol, hypertension, diabetes or PVD
- High blood pressure or hypertension: An established association exists between high blood pressure PVD. The risk of PVD may be higher by up to two times in persons with hypertension
- Smoking: Use of tobacco in any form is one of the highest-ranked risk factors for PVD across the world. It is estimated that smoking tobacco may increase the PVD risk of a person up to 10 times. Not just active smoking, but also second-hand or passive smoking can lead to PVD changes in blood vessels of a person that may cause atherosclerosis. It is observed that approximately 90% of persons having lower extremity PVD had a history of smoking or actively smoke.
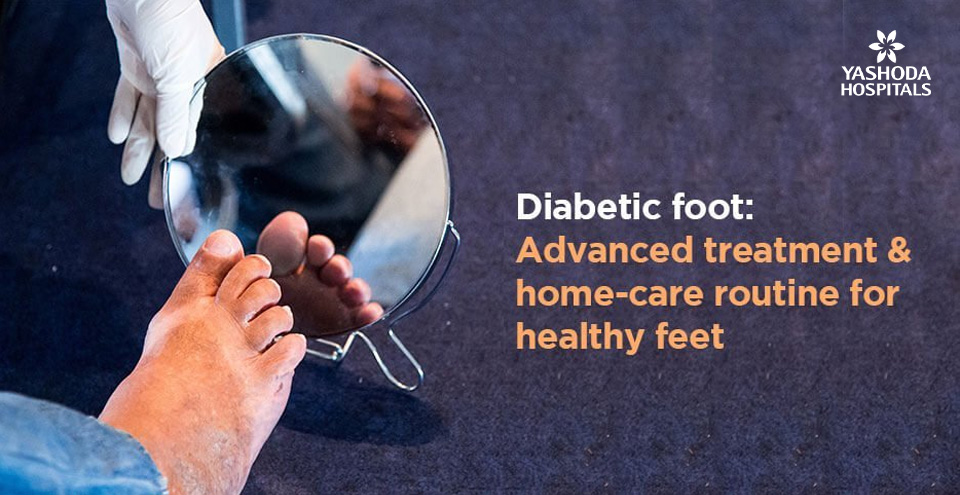
- Uncontrolled blood sugar: Individuals suffering from diabetes are likely to have a higher risk of PVD. Uncontrolled blood sugar increases this risk further, which may be as high as two to four times. The prolonged uncontrolled blood sugar level in the body leads to changes in the cells of the lining and smooth muscles of the blood vessels, thereby increasing their risk for atherosclerosis.
- Weight: Obese persons are more likely to have PVD
What are the symptoms of peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
The presence of PVD in many cases may not be evident due to mild or no symptoms. In some persons, it may be reported as leg pain when walking (also called as claudication). Some characteristics of claudication are:
- Muscle pain or cramping in the legs or arms aggravated by physical activity like walking which disappears after resting for some time.
- Though calf pain is the most common location, the location of the pain indicates the location of the narrowed artery.
- The severity of claudication is a variable that can range from mild discomfort to severe restrictive pain that can interfere with physical activity.
Some of the other commonly reported signs and symptoms of PVD include:
- Change in color of the skin of the limb
- Coldness in the affected limb
- Erectile dysfunction in men
- The glossy or shiny surface of the skin of the affected limb
- Non-healing sores or ulcers on the toes, feet or legs
- Numbness or weakness of the limb, especially the legs
- Poor growth of hair and nails of the affected limb
Severe progression of the PVD may lead to pain at rest or while lying down.
How to diagnose peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
A detailed medical history and physical examination can help a doctor to make an initial diagnosis of PVD or PAD.
-
Physical examination: Presence of weak or absent pulse in the suspected area, bruits (murmur) or whooshing sounds heard with a stethoscope over the affected blood vessel, observation of skin texture, delayed healing of ulcers, etc are made note of.
The initial diagnosis is confirmed by certain specialized tests that include:
- Ankle-brachial index (ABI): A comparison of the blood pressure in the ankle with the blood pressure in the person’s arm is done using a regular blood pressure cuff and an ultrasound device.
- Angiography: This test is performed to observe the blood flow through the blood vessels in real-time by using a contrast material or dye that is injected into the blood vessel. The contrast material can be observed using imaging techniques, such as X-ray, computerized tomography angiography (CTA) or magnetic resonance angiography (MRA). Any evidence of cutoff of blood supply in the limbs may be due to blockage as in PAD.

A more invasive form of this test is the catheter angiography in which a guiding catheter is advanced through an artery of the groin to the affected area. The dye is injected through the catheter route. Treatment if required can be simultaneously performed in this technique.
- Blood tests: A sample of your blood can be used to measure your cholesterol and triglycerides and to check for diabetes.
- Doppler ultrasound: An imaging technique with specialized ultrasound helps the doctor in evaluating the blood flow through the blood vessel to identify the area of blockage.
What are the stages of peripheral vascular disease?
There are two most commonly recommended methods to determine the stage of PVD. Introduced by René Fontaine in 1954, the Fontaine stages define the severity of PVD
-
Stage I: Asymptomatic
Most of the time the person is asymptomatic but have specific, subtle symptoms, like paresthesia. Presence of cold extremities, reduced peripheral pulse or murmurs in the peripheral arteries are noticable upon examination.
-
Stage II: Presence of Intermittent claudication.
The pain appears at a constant distance
Stage IIa – Intermittent claudication after more than 200 m of walking.
Stage IIb – Intermittent claudication after less than 200 m of walking. -
Stage III – Rest pain
Pain may appear at rest, especially during the night while the legs are raised and may disappear during the day.
- Stage IV – Ischaemic ulcers or gangrene (dry or humid)
The Society for Vascular Surgery introduced the Rutherford classification after the Robert B. Rutherford, an American vascular surgeon
The Rutherford classification describes seven stages of peripheral artery disease:
- Stage 0: Asymptomatic.
- Stage 1: Mild claudication.
- Stage 2: Moderate claudication – the distance that delineates mild, moderate, and severe claudication are not specified in the Rutherford classification, as it is in the Fontaine classification.
- Stage 3: Severe claudication.
- Stage 4: Rest pain.
- Stage 5: Ischemic ulceration not exceeding ulcers of the digits of the foot.
- Stage 6: Severe ischemic ulcers or frank gangrene.
What can be the complications of peripheral artery disease?
Undiagnosed and untreated peripheral artery disease can lead to serious and sometimes even life-threatening complications. The presence of PVD in a specific site can also be a warning sign of the presence of generalized vascular disease.
Some of the common complications of untreated peripheral artery disease are:
- Death of tissue or gangrene that may sometimes lead to limb amputation
- Impotence
- Severe pain that restricts physical activity
- Non-healing ulcers
- Spread of life-threatening infections into the bones and bloodstream
- One of the most serious complications of PVD is the blockage of blood vessels of the heart that can cause heart attack, stroke, or even death.
How to treat peripheral artery disease (PAD) or peripheral vascular disease (PVD)?
The treatment for peripheral artery disease has two major objectives:
- Management of symptoms like leg pain to restore a good quality of life.
- Prevent the progression of the pathology like atherosclerosis in the other blood vessels to reduce a person’s risk of other complications like heart attack and stroke
These goals can be achieved by a combination of lifestyle changes, medications, and surgical management depending on the severity.
Lifestyle management
- Elimination of modifiable risk factors like stopping smoking
- Regular physical exercise helps in opening up of alternative small vessels that provide collateral blood flow and prevent limitation of physical activity.
Medication management: Any existing medical conditions should be managed with medications and periodically reviewed by treating physicians. These may include but are not limited to the following categories of medications :
- Cholesterol-lowering
- Blood pressure
- Blood sugar
- Blood thinners to prevent blood clots
- Pain killers
Surgical management: Cases, where claudication and ischemia are not relieved by conservative management, patient may be considered for revascularization with angioplasty and bypass by a vascular or endovascular surgeon.
Angioplasty: A catheter which is essentially a hollow tube with a balloon at the tip is inserted through a blood vessel into the affected artery. Once the affected site is reached, the balloon is inflated. The inflation of the balloon reopens the artery and flattens the blockage into the wall of the artery. The blood flow increases due to the simultaneous stretching and opening up of the artery. A mesh framework known as a stent is placed in the artery to maintain the opening, a procedure similar to angioplasty of the heart arteries.

Bypass surgery: If the blockage is not amenable to angioplasty, the surgeon may create a bypass for the blockage site using a graft from a vessel in another part of the person’s body. Sometimes a synthetic graft may be used. Following this technique, the flow of the blood “bypasses” the affected area and normal circulation are restored.
Atherectomy: Sometimes, normal blood flow from the affected site in the blood vessel may be restored by surgically scraping off the plaque off of the inside of the vessel wall
Amputation: Severe cases where gangrene has set in beyond repair, the limb may have to be surgically cut off to prevent the infection from spreading into the body
Thrombolytic therapy: If an artery gets blocked due to a clot, an injection of a clot-dissolving drug may be administered into the artery at the point of the clot to break it up into smaller fragments.
How to prevent peripheral artery disease?
Maintaining a healthy lifestyle is by far the most important way to prevent PVD since many of its risk factors are related to a person’s lifestyle. Some of the important preventive measures are:
- Avoid second-hand smoke and stop active smoking if you do.
- Manage your medical condition well if you have been diagnosed with any like diabetes, hypertension, etc.
- Exercise regularly after consulting your physician if you have a medical condition.
- Have a healthy diet and eat foods that are low in saturated fat.
- Maintain a healthy weight.
Conclusion
With the advancement in medical technology, newer treatment options have emerged for PVD in the field of peripheral intervention. A marked increase in the understanding of the disease dynamics and treatment methodologies has also led to a dramatic improvement in the quality of consumables and devices like balloons, stents, devices for atherectomy, etc. Newer consumables like drug-eluting stents and balloons help in durable and long-term treatment outcomes. As a result, the recurrence rate and postoperative complications decrease. Alternative techniques like atherectomy in cases where stents are not recommended are proving to be of benefit in many cases. Drug-eluting balloons combined with atherectomy have also shown satisfactory results in many reported studies. Considering the difference in the anatomy and physiology of the limbs and heart where the angioplasty procedure is now the proven standard of care, advanced technology stents that are suitable to the peripheral vessels are now available. However, it should be emphasized that the management of PVD is an intensive team effort that requires a multidisciplinary approach consisting of specialists from areas of vascular surgery, interventional cardiology, radiology, endocrinology, diabetologists, and trained paramedical staff. Further advanced medical infrastructure also must provide comprehensive care for the limbs at risk. Hence it is recommended that care for PVD should be considered at a multispecialty centre of excellence.
References:
-
https://www.healthline.com/health/peripheral-vascular-disease#prevention
-
Mayo Clinic. Peripheral artery disease. Available at: https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557. Accessed on December 17, 2019
-
Johns Hopkins Medicine.Peripheral Vascular Disease. https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-vascular-disease Accessed on December 17, 2019
-
Society for vascular surgery. Peripheral Arterial Disease. Available at: https://vascular.org/patient-resources/vascular-conditions/peripheral-arterial-disease. Accessed on December 17, 2019











 Appointment
Appointment Second Opinion
Second Opinion WhatsApp
WhatsApp Call
Call More
More





